Fill Out a Valid Biopsychosocial Assessment Social Work Form
The Biopsychosocial Assessment Social Work form is a comprehensive tool designed to gather essential information about an individual's mental, emotional, and physical health. This form aims to provide a holistic view of a person's life circumstances, integrating biological, psychological, and social factors that may influence their well-being. At the outset, clients are asked to share their presenting problems, including how long they have been experiencing these issues and their intensity. This section is crucial, as it sets the stage for understanding the client’s immediate needs and therapeutic goals. Additionally, the form delves into various aspects of the client's life, such as their substance use history, family dynamics, educational background, and legal issues. It also addresses current health concerns, including any past trauma or mental health treatment. By exploring these dimensions, social workers can better understand the complexities of each client's situation, fostering a more personalized approach to care. Throughout the process, clients are encouraged to provide as much detail as they feel comfortable with, ensuring that their unique experiences and challenges are acknowledged and respected.
Common mistakes
-
Incomplete Information: Failing to fill out all sections of the form can lead to gaps in understanding your situation. Each question is important for a comprehensive assessment.
-
Rushed Responses: Providing hasty answers may result in missing important details. Take your time to reflect on each question to ensure clarity.
-
Skipping Sensitive Questions: Avoiding questions about trauma or mental health can hinder the assessment process. It’s crucial to be open for accurate support.
-
Not Disclosing Current Medications: Omitting information about medications can affect treatment recommendations. Include all medications, even over-the-counter ones.
-
Neglecting to Mention Past Experiences: Past traumas or significant life events shape current challenges. Share relevant experiences to provide context.
-
Misunderstanding Terminology: Some terms may be confusing. If unsure about a question, ask for clarification instead of guessing.
-
Ignoring Family History: Family dynamics and history of mental health issues are significant. Include this information to help identify patterns.
-
Not Being Honest: Withholding or altering information can lead to ineffective treatment. Honesty is vital for receiving the best care possible.
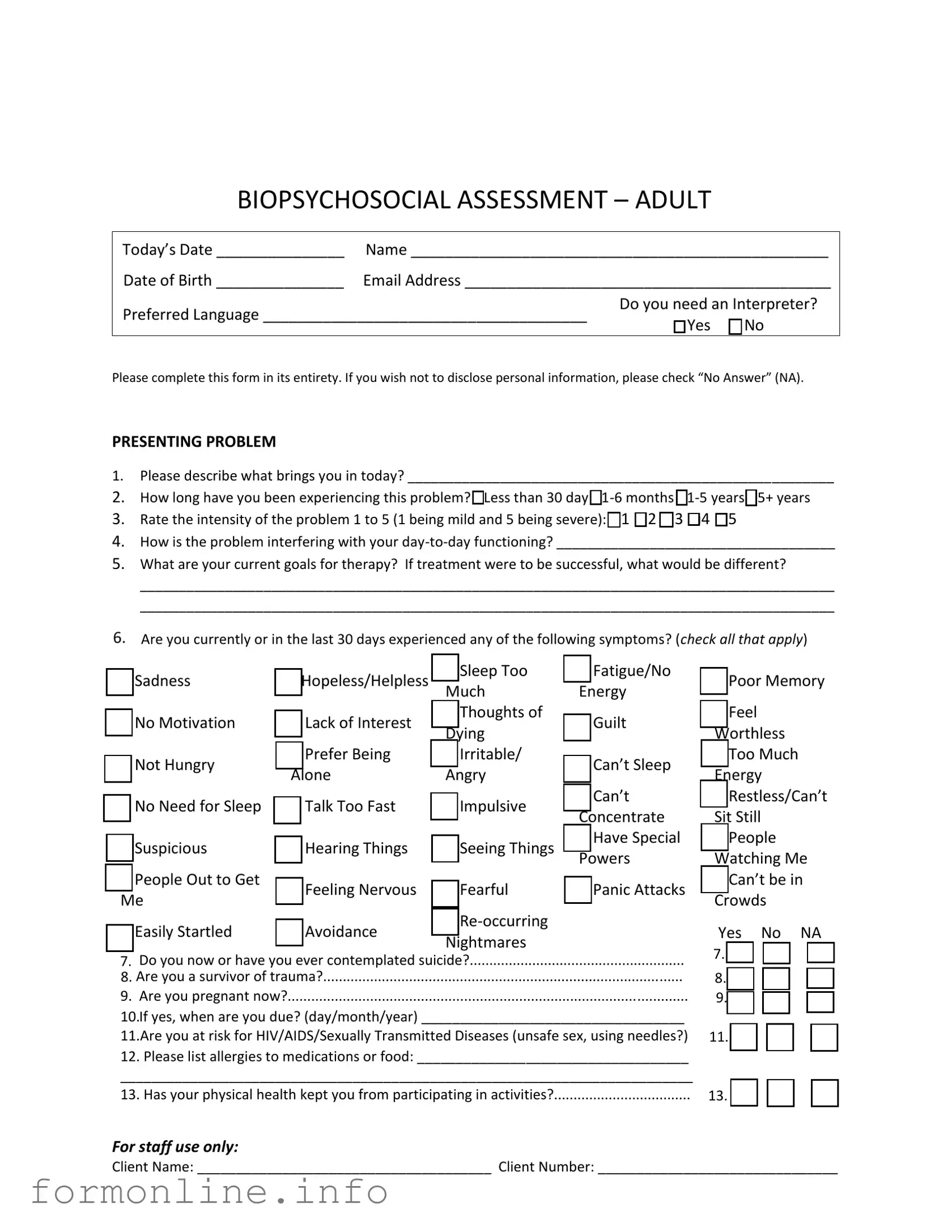
Preview - Biopsychosocial Assessment Social Work Form
BIOPSYCHOSOCIAL ASSESSMENT – ADULT
Today’s Date _______________ |
Name _________________________________________________ |
Date of Birth _______________ |
Email Address ___________________________________________ |
Preferred Language ______________________________________ |
Do you need an Interpreter? |
|
□ Yes □ No |
||
|
Please complete this form in its entirety. If you wish not to disclose personal information, please check “No Answer” (NA).
PRESENTING PROBLEM
1.Please describe what brings you in today? _______________________________________________________
2.How long have you been experiencing this problem? □Less than 30 day
3.Rate the intensity of the problem 1 to 5 (1 being mild and 5 being severe): □1 □2 □3 □4 □5
4.How is the problem interfering with your
5.What are your current goals for therapy? If treatment were to be successful, what would be different?
__________________________________________________________________________________________
__________________________________________________________________________________________
6.Are you currently or in the last 30 days experienced any of the following symptoms? (check all that apply)
□Sadness
□No Motivation
□Not Hungry
□No Need for Sleep
□Suspicious
□People Out to Get
Me
□Easily Startled
□Hopeless/Helpless |
□ Sleep Too |
□ Fatigue/No |
|
|
Much |
Energy |
|
□ Lack of Interest |
□ Thoughts of |
□ Guilt |
|
Dying |
|||
|
|
||
□ Prefer Being |
□ Irritable/ |
□ Can’t Sleep |
|
Alone |
Angry |
||
|
|||
□ Talk Too Fast |
□ Impulsive |
□ Can’t |
|
Concentrate |
|||
|
|
||
□ Hearing Things |
□ Seeing Things |
□ Have Special |
|
Powers |
|||
|
|
||
□ Feeling Nervous |
□ Fearful |
□ Panic Attacks |
|
□ Avoidance |
□ |
|
|
Nightmares |
|
||
|
|
□Poor Memory
□Feel
Worthless
□Too Much
Energy
□Restless/Can’t
Sit Still
□People
Watching Me
□Can’t be in Crowds
Yes No NA |
7. Do you now or have you ever contemplated suicide?.......................................................
8. Are you a survivor of trauma?............................................................................................
9. Are you pregnant now?......................................................................................................
10.If yes, when are you due? (day/month/year) __________________________________
11.Are you at risk for HIV/AIDS/Sexually Transmitted Diseases (unsafe sex, using needles?)
12. Please list allergies to medications or food: ___________________________________
__________________________________________________________________________
13. Has your physical health kept you from participating in activities?...................................
7. |
□ |
□ |
□ |
8. |
□ |
□ |
□ |
9. |
□ |
□ |
□ |
11. |
□ |
□ |
□ |
13. |
□ |
□ |
□ |
For staff use only:
Client Name: ______________________________________ Client Number: _______________________________
TOBACCO |
|
Yes |
No |
NA |
1. Have you ever used any forms of tobacco (cigarettes, snuff, etc.)? IF NO SKIP TO NEXT |
1. |
□ |
□ |
□ |
SECTION……………………………………………………………………………………………………………………………… |
|
|
|
|
2. Are you a former tobacco user? |
2. |
□ |
□ |
□ |
3.If yes, what form(s) of tobacco have you used in the past (please check all that apply)
□ Cigarettes □ Cigars □ Snuff □ Chewing Tobacco □ Snuff □ Other
4.How many times on an average day do you use tobacco
Cigarettes____ Cigars____ Snuff____ Chewing Tobacco____ Snuff____ |
|
|
|
|
5. Have you been involved in a program to help you quit using tobacco in the past 30 |
5. |
□ |
□ |
□ |
days? |
|
|
|
|
6. If so, which |
|
|
|
|
SUBSTANCE USE/ADDICTION PRESENT |
|
Yes |
No |
NA |
1. Would you or someone you know say you are having a problem with alcohol?......………… |
1. |
□ |
□ |
□ |
2. Would you or someone you know say you are having problems with pills or illegal |
2. |
□ |
□ |
□ |
drugs? |
|
|
|
|
3. Would you or someone you know say you are having problems with other addictions, ie. |
3. |
□ |
□ |
□ |
gambling, pornography or shopping? |
|
|
|
|
4. Have you ever been to a |
4. |
□ |
□ |
□ |
SUBSTANCE USE/ADDICTION PAST |
|
Yes |
No |
NA |
1. Would you or someone you know say you had a problem with alcohol?......…………………… |
1. |
□ |
□ |
□ |
2. Would you or someone you know say you had problems with pills or illegal drugs? |
2. |
□ |
□ |
□ |
3. Would you or someone you know say you had problems with other addictions, ie. |
3. |
□ |
□ |
□ |
gambling, pornography or shopping? |
|
|
|
|
4. Is there a family history of addiction in your family? |
4. |
□ |
□ |
□ |
5. If yes, please describe: _____________________________________________________ |
|
|
|
|
PERSONAL, FAMILY AND RELATIONSHIPS |
|
Yes |
No |
NA |
1.Who is in your family? (parents, brothers, sisters, children, etc.)____________________
__________________________________________________________________________
2. |
Has there been any significant person or family member enter or leave your life in the |
2. □ |
□ |
□ |
|||||
last 90 days? |
|
|
|
|
|
|
|||
|
|
Good Fair Poor Close Stressful Distant Other |
|||||||
3. |
How are the relationships in your family? |
□ |
□ |
□ |
□ |
□ |
□ |
□ |
|
4. |
How are the relationships in your support system (friends, |
□ |
□ |
□ |
□ |
□ |
□ |
□ |
|
extended family, et.?)………………………………………………………………. |
|||||||||
|
|
|
|
|
|
|
|||
|
|
|
|
Conflict Abuse Stress Loss Other |
|||||
5. |
Are there any problems in your family now? (check all that apply)………….. |
□ |
□ |
□ |
□ |
□ |
|||
6. |
Were there any problems with your family in the past? (check all that |
|
□ |
□ |
□ |
□ |
□ |
||
apply)…………………………………………………………………………………………………………... |
|
|
|
|
|
||||
7. Are there any problems in your support system now? (check all that |
|
□ |
□ |
□ |
□ |
□ |
|||
apply)…………………………………………………………………………………………………………… |
|
|
|
|
|
||||
8. Were there any problems with your support system in the past? (check |
□ |
□ |
□ |
□ |
□ |
||||
all that apply)………………………………………………………………………………………………. |
|
|
|
|
|
||||
9.What is your marital status now? □Single □Married □Living as Married □Divorced □Widowed □Never Married
For staff use only:
Client Name: ______________________________________ Client Number: _______________________________
10.Have you ever had problems with marriage/relationships?..............................................
11.If yes, please check why: □Stress □Conflict □Loss □Divorced/Separation
□Trust Issues □Other_______________________________
12.Do you have any close friends?..........................................................................................
13.Do you have problems with friendships?...........................................................................
14.Do you get along well with others (neighbors,
15.What do you like to do for fun? _____________________________________________
Yes |
No |
NA |
10. □ |
□ |
□ |
12. □ |
□ |
□ |
13. □ |
□ |
□ |
14. □ |
□ |
□ |
EDUCATION
1.What is the highest grad you completed in school? (please check)
□No Education
2.Would you describe your school experience as positive or negative?________________
3.Are you currently in school or a training program?..............................................................
Yes No NA
3. □ □ |
□ |
LEGAL
1.Have you ever been arrested? IF NO SKIP TO NEXT SECTION………………………………………….
2.In the past month?...............................................................................................................
3.If yes, how many times? ____________________________________________________
4.In the past year?...................................................................................................................
5.If yes, how many times? ____________________________________________________
6.If yes, what were you arrested for? ___________________________________________
7.What was the name of your attorney? ________________________________________
8.Were you ever sentenced for a crime?…………………………………………………………………………….
9.If yes, number of prison sentences served? ____________________________________
10.What year(s) did this occur? _______________________________________________
11.Are you currently or have you ever been on probation or parole?....................................
12.If yes, what is the name of your attorney or probation officer? ____________________
WORK
1.What is your work history like? □Good □Poor □Sporadic □Other
2.How long do you normally keep a job? □Weeks □Months □Years
3.Are you retired?....................................................................................................................
4.If yes, what kind of work do you do/did you do in the past? _______________________
5.Have you ever served in the military?..................................................................................
6.If yes, are you: □Active □Retired □Other
|
Yes |
No |
NA |
1. |
□ |
□ |
□ |
2. |
□ |
□ |
□ |
4. |
□ |
□ |
□ |
8. |
□ |
□ |
□ |
11. □ |
□ |
□ |
|
|
Yes |
No |
NA |
3. |
□ |
□ |
□ |
5. |
□ |
□ |
□ |
MEDICAL
1.Current Primary Care Physician: __________________________________Phone_________________
2.Past and Current Medical/Surgical Problems: _____________________________________________
3.Past and Current Medications and Dosages: ______________________________________________
__________________________________________________________________________________
4. Have you seen a Mental Health Professional Before? □ Yes □ No
5.If yes, Name, When, and Reason for Changing: ____________________________________________
6.Current Psychiatrist/APRN, if applicable:_________________________________________________
7.Is there anything else you would like me to know about you?_______________________________
__________________________________________________________________________________
For staff use only:
Client Name: ______________________________________ Client Number: _______________________________
Other PDF Templates
Flea Tick Certificate - Veterinarians are responsible for the accuracy of the health examination statement.
Obtaining a thorough guide to Power of Attorney for a Child is crucial for parents who want to ensure their child's wellbeing in their absence. This specific legal document provides the necessary authority for a designated caregiver to make important decisions when needed.
Ucc 308 Without Prejudice - It allows you to publicly declare your status to interested parties.
Documents used along the form
The Biopsychosocial Assessment is a crucial tool in social work, providing a comprehensive view of an individual's mental, emotional, and social well-being. Alongside this assessment, several other forms and documents are commonly utilized to gather additional information, ensure continuity of care, and support effective treatment planning. Below is a list of documents that are often used in conjunction with the Biopsychosocial Assessment.
- Intake Form: This document collects essential demographic information, contact details, and basic medical history. It serves as the first step in understanding a client's background and needs.
- Release of Information (ROI): This form authorizes the sharing of a client’s personal health information with other professionals or organizations. It is vital for coordinating care and ensuring that all parties involved have the necessary information.
- Treatment Plan: Following the assessment, a treatment plan outlines the goals, interventions, and expected outcomes for the client's care. It serves as a roadmap for both the client and the social worker.
- Progress Notes: These notes document each session's discussions, interventions, and client progress. They are essential for tracking changes over time and adjusting treatment as needed.
- Texas Motorcycle Bill of Sale: This legal document records the transaction between a seller and a buyer for the transfer of ownership of a motorcycle in Texas. To ensure proper documentation, you can print the document easily.
- Safety Plan: For clients at risk of self-harm or harm to others, a safety plan provides strategies and resources to manage crises. It includes emergency contacts and coping strategies to ensure the client’s safety.
- Referral Form: When a client needs services outside the social worker's expertise, a referral form is used to connect them with appropriate resources. This helps in addressing specific needs, such as substance abuse treatment or housing assistance.
These documents collectively enhance the assessment process, ensuring that social workers have a holistic understanding of their clients. By integrating various forms of information, social workers can provide tailored support and interventions that meet the unique needs of each individual.
Similar forms
The Biopsychosocial Assessment Social Work form shares similarities with the Mental Health Intake Form, which serves as a foundational document in mental health treatment. Both forms aim to gather comprehensive information about an individual’s psychological, social, and biological factors affecting their well-being. The Mental Health Intake Form typically includes questions about the individual's presenting issues, history of mental health treatment, and family background. Like the Biopsychosocial Assessment, it seeks to create a holistic picture of the client, allowing mental health professionals to tailor their interventions effectively.
In the realm of legal documents, the importance of clarity and precision cannot be overstated, especially when drafting a Last Will. This instrument ensures that a person's wishes regarding the distribution of their assets after death are honored, offering peace of mind to both the testator and their beneficiaries. By providing clear directives, it prevents disputes and ambiguities that may arise, allowing the estate to be settled in accordance with the deceased's intentions.
Another document comparable to the Biopsychosocial Assessment is the Substance Abuse Assessment form. This form is specifically focused on understanding an individual's relationship with substances, including alcohol and drugs. Both assessments delve into the client's history and current use patterns, helping to identify any potential dependencies or issues. By exploring similar themes, such as the impact of substance use on daily functioning and relationships, both documents aim to inform treatment planning and support recovery efforts.
The Family Assessment form also bears resemblance to the Biopsychosocial Assessment. This document focuses on the dynamics within a client's family system, exploring relationships, conflicts, and support structures. While the Biopsychosocial Assessment takes a broader view, incorporating personal, social, and medical histories, the Family Assessment zooms in on interpersonal relationships. Both forms recognize the critical role of family and social support in an individual’s overall health, making them vital tools for social workers and therapists.
Lastly, the Health History form is similar to the Biopsychosocial Assessment in that it collects detailed information about an individual's medical background. This document typically includes inquiries about past medical conditions, surgeries, and current medications. Just as the Biopsychosocial Assessment considers physical health as a component of overall well-being, the Health History form provides essential context for understanding how physical health may intersect with psychological and social factors. Together, these documents create a comprehensive view of an individual's health, aiding in more effective treatment planning.
Dos and Don'ts
When filling out the Biopsychosocial Assessment Social Work form, consider the following guidelines:
- Be honest and thorough in your responses. This information is crucial for effective support.
- Take your time to reflect on each question. Rushing may lead to incomplete or inaccurate answers.
- Use "No Answer" (NA) for questions you prefer not to disclose. This is perfectly acceptable.
- Clearly describe your presenting problem. Specific details can help your therapist understand your situation better.
- Rate the intensity of your problem honestly. This helps in assessing the urgency of your needs.
- List any current medications or allergies accurately. This information is vital for your safety and treatment.
- Ask for help if you don’t understand a question. It's important to provide the best information possible.
Conversely, avoid the following pitfalls:
- Do not leave questions blank unless you choose "No Answer." Incomplete forms can delay your assessment.
- Avoid exaggerating or downplaying your symptoms. Accuracy is key for effective treatment.
- Do not provide vague answers. Specificity will aid your social worker in understanding your needs.
- Refrain from using jargon or technical terms. Clear communication is essential.
- Do not rush through the form. Take the necessary time to think about your responses.
- Do not hesitate to express concerns or ask for clarification on any part of the form.
- Do not feel pressured to share more than you are comfortable with. Your privacy is important.
Key takeaways
Filling out the Biopsychosocial Assessment Social Work form is an important step in understanding an individual's needs. Here are some key takeaways to keep in mind:
- Complete the form fully. Providing detailed information helps professionals better understand your situation.
- Be honest about your presenting problem. Clearly describe what brings you in today to ensure you receive the appropriate support.
- Rate the intensity of your problem. Use the scale provided to indicate how severe your issue feels to you.
- Discuss your goals for therapy. Sharing what you hope to achieve can guide the treatment process effectively.
- Indicate any symptoms you are experiencing. Mark all that apply to give a complete picture of your mental health.
- Consider your support system. Reflect on your relationships with family and friends, as these can impact your well-being.
- Be open about your medical history. Include any past or current health issues, medications, and treatments.
- Don’t hesitate to ask for help. If you need assistance with the form or have questions, reach out to the staff for support.
How to Use Biopsychosocial Assessment Social Work
Filling out the Biopsychosocial Assessment Social Work form is an important step in understanding your current situation and needs. This form allows you to share information about various aspects of your life, including your mental health, relationships, and medical history. To ensure a smooth process, follow these steps carefully.
- Gather Your Information: Before you start, make sure you have all necessary details handy, such as your name, date of birth, email address, and preferred language.
- Today’s Date: Write today’s date at the top of the form.
- Personal Information: Fill in your name, date of birth, email address, and preferred language. Indicate if you need an interpreter.
- Presenting Problem: Answer the questions about what brings you in today, how long you’ve been experiencing the problem, and how it affects your daily life. Rate the intensity of the problem from 1 to 5.
- Current Goals: Describe your goals for therapy and what success would look like for you.
- Symptoms: Check all symptoms you have experienced in the last 30 days. If applicable, answer questions about suicidal thoughts and trauma history.
- Pregnancy and Health Risks: Indicate if you are pregnant and when you are due. Also, mention any risks for HIV/AIDS or STDs, and list any allergies.
- Tobacco Use: Answer questions about your tobacco use history and current habits.
- Substance Use/Addiction: Respond to questions regarding any current or past issues with alcohol, drugs, or other addictions.
- Personal, Family, and Relationships: Provide details about your family, significant relationships, and any current or past issues within these relationships.
- Education: Indicate your highest level of education and describe your school experience.
- Legal History: Answer questions about any arrests or legal issues you may have faced.
- Work History: Describe your work history, including job stability and military service if applicable.
- Medical History: Provide information about your primary care physician, any medical issues, medications, and mental health professionals you have seen.
- Final Thoughts: If there is anything else you would like to share, write it in the designated area.
Once you have completed the form, review your answers for accuracy. This information will help your social worker understand your unique situation and tailor their support to meet your needs.