Fill Out a Valid Certification Of Incapacity Form
The Certification of Incapacity form is a crucial document in the healthcare process, particularly when patients are unable to make informed decisions regarding their medical treatment. This form requires the assessment and certification from two physicians, establishing that a patient lacks the capacity to understand or evaluate the implications of proposed medical interventions. Each physician must provide details about their examination of the patient, including the date and time, and specify the medical treatments in question. The form also necessitates a clear explanation of the patient's condition that contributes to their incapacity, highlighting whether they cannot comprehend the nature or consequences of the treatment or if they are unable to communicate their decisions. Timeliness is essential; one of the physicians must complete their certification within two hours of the examination to ensure the accuracy and relevance of the assessment. This process aims to protect patients' rights and ensure that their medical care is handled with the utmost respect and consideration.
Common mistakes
-
Not filling in the patient's name correctly. Make sure the name matches official documents.
-
Forgetting to include the date and time of the examination. This information is crucial for validation.
-
Leaving the section about the patient's condition blank. This should clearly explain why the patient is incapacitated.
-
Not checking one of the options regarding the patient's ability to make decisions. Always select either the evaluation or communication option.
-
Failing to note if the attestation was made within the required two-hour timeframe. This is essential for compliance.
-
Not having the second physician's certification completed if required. This step is often necessary for validation.
-
Overlooking the signature of the attending physician. An unsigned form may not be accepted.
-
Using abbreviations or jargon that might confuse others. Keep the language clear and straightforward.
-
Neglecting to provide a clear description of the proposed treatment. This should be detailed enough for understanding.
-
Not keeping a copy of the completed form for personal records. It's important to have documentation for future reference.
Preview - Certification Of Incapacity Form

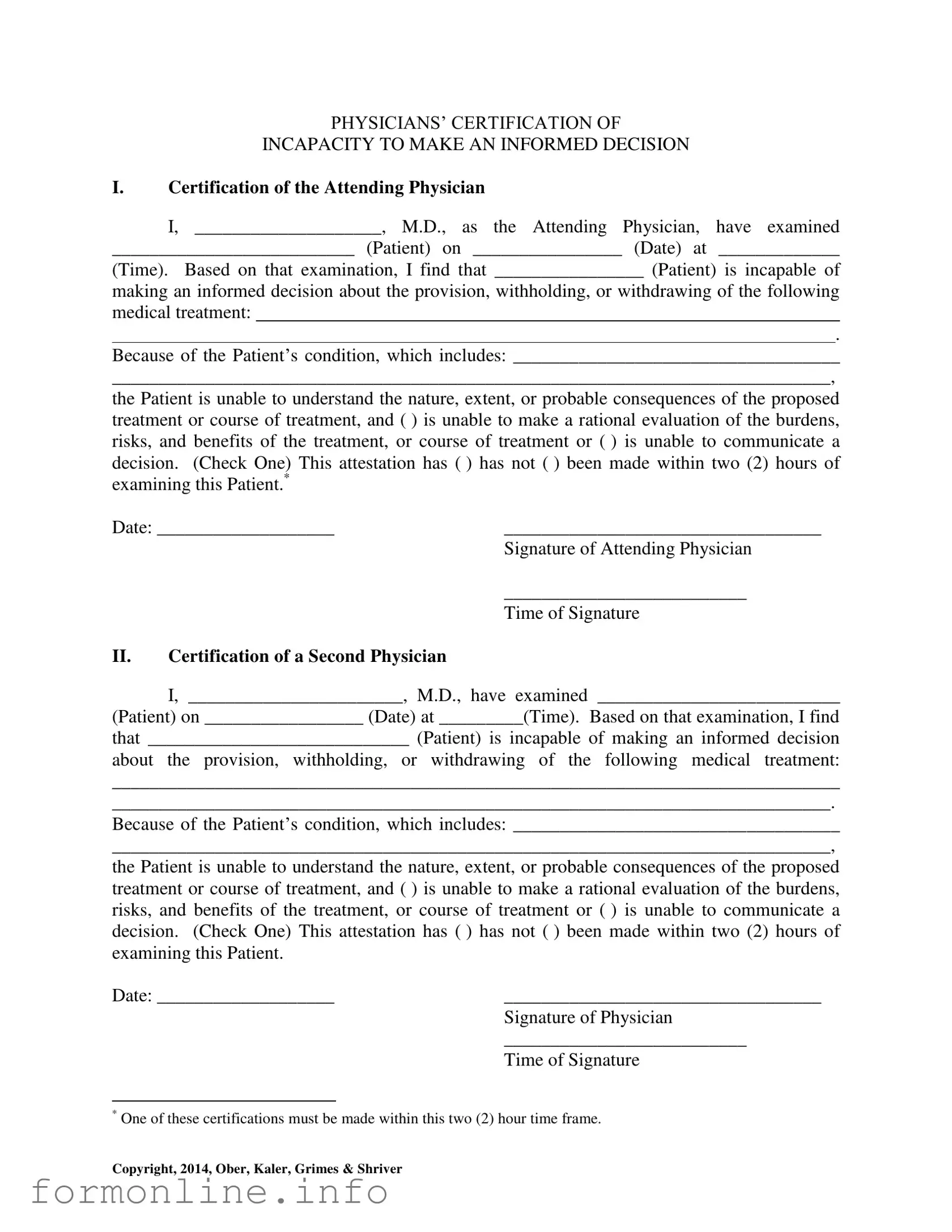
PHYSICIANS’ CERTIFICATION OF
INCAPACITY TO MAKE AN INFORMED DECISION
I.Certification of the Attending Physician
I, ____________________, M.D., as the Attending Physician, have examined
__________________________ (Patient) on ________________ (Date) at _____________
(Time). Based on that examination, I find that ________________ (Patient) is incapable of
making an informed decision about the provision, withholding, or withdrawing of the following medical treatment:
.
Because of the Patient’s condition, which includes: ___________________________________
_____________________________________________________________________________,
the Patient is unable to understand the nature, extent, or probable consequences of the proposed treatment or course of treatment, and ( ) is unable to make a rational evaluation of the burdens, risks, and benefits of the treatment, or course of treatment or ( ) is unable to communicate a decision. (Check One) This attestation has ( ) has not ( ) been made within two (2) hours of examining this Patient.*
Date: ___________________ |
__________________________________ |
|
Signature of Attending Physician |
|
__________________________ |
|
Time of Signature |
II.Certification of a Second Physician
I, _______________________, M.D., have examined __________________________
(Patient) on _________________ (Date) at _________(Time). Based on that examination, I find
that ____________________________ (Patient) is incapable of making an informed decision
about the provision, withholding, or withdrawing of the following medical treatment:
______________________________________________________________________________
_____________________________________________________________________________.
Because of the Patient’s condition, which includes: ___________________________________
_____________________________________________________________________________,
the Patient is unable to understand the nature, extent, or probable consequences of the proposed treatment or course of treatment, and ( ) is unable to make a rational evaluation of the burdens, risks, and benefits of the treatment, or course of treatment or ( ) is unable to communicate a decision. (Check One) This attestation has ( ) has not ( ) been made within two (2) hours of examining this Patient.
Date: ___________________ |
__________________________________ |
|
Signature of Physician |
|
__________________________ |
|
Time of Signature |
*One of these certifications must be made within this two (2) hour time frame.
Copyright, 2014, Ober, Kaler, Grimes & Shriver
Other PDF Templates
Air Force Award Form - The AF 1206 may be used for various awards, tailoring details to fit specific criteria.
The Employment Verification process is crucial for employers aiming to validate an employee's work history and present credentials. For a thorough guide, the form provided can be referenced in relation to the important Employment Verification requirements that are essential in many professional settings.
Dol - A resource explaining how to obtain information on labor disputes and resolutions.
Documents used along the form
The Certification of Incapacity form is a vital document in the healthcare field, particularly when it comes to ensuring that individuals who are unable to make informed decisions about their medical care are adequately protected. However, this form often exists alongside several other important documents that help clarify the patient's wishes, establish legal authority, or provide additional context regarding their medical condition. Below is a list of commonly used forms and documents that may accompany the Certification of Incapacity.
- Durable Power of Attorney for Healthcare: This document allows a person to appoint someone else to make healthcare decisions on their behalf if they become incapacitated. It ensures that the appointed individual can act according to the patient's wishes.
- Living Will: A living will is a written statement detailing a person's preferences regarding medical treatment in situations where they cannot communicate their wishes. It typically addresses end-of-life care and other critical medical decisions.
- Advance Healthcare Directive: This comprehensive document combines elements of both a durable power of attorney and a living will. It outlines a person's healthcare preferences and designates an agent to make decisions if the individual is unable to do so.
- Physician Orders for Life-Sustaining Treatment (POLST): This form translates a patient's wishes regarding life-sustaining treatment into actionable medical orders. It is especially useful for patients with serious illnesses and ensures that their preferences are honored in emergencies.
- Medical History Form: This document provides healthcare providers with a comprehensive overview of a patient's medical history, including previous illnesses, surgeries, medications, and allergies. It is essential for informed decision-making.
- Consent for Treatment: This form is used to obtain a patient's consent for specific medical procedures or treatments. If a patient is incapacitated, a designated decision-maker may need to provide consent on their behalf.
- Patient Rights and Responsibilities Document: This document outlines the rights of patients regarding their care and treatment, as well as their responsibilities. It serves to inform patients and their families about what they can expect in a healthcare setting.
- Care Plan: A care plan details the medical and therapeutic strategies to be employed for a patient. It is essential for coordinating care among various healthcare providers and ensuring that the patient's needs are met.
- Guardian Ad Litem Appointment: In some cases, a court may appoint a guardian ad litem to represent the interests of an incapacitated individual. This document formalizes that appointment and outlines the guardian's responsibilities.
- Virginia Homeschool Letter of Intent: This important document must be submitted to inform the local school division of the family's intention to homeschool, ensuring a proper start to the homeschooling process. For more details, you can refer to the Homeschool Letter of Intent.
- Notice of Rights: This document informs patients and their families about their legal rights in the healthcare system, including the right to refuse treatment and the right to privacy regarding their medical information.
Understanding these documents is crucial for both patients and their families. Each plays a unique role in ensuring that medical care aligns with the patient's wishes and legal rights, particularly in situations where the individual is unable to advocate for themselves. By familiarizing oneself with these forms, individuals can better navigate the complexities of healthcare decisions and ensure that their or their loved ones' preferences are respected.
Similar forms
The Advance Directive is a crucial document that allows individuals to outline their preferences for medical treatment in case they become unable to communicate their wishes. Similar to the Certification of Incapacity, it requires a clear understanding of the individual’s health status and treatment options. Both documents serve to protect the rights and desires of patients, ensuring that their treatment aligns with their values, even when they cannot voice them. The Advance Directive can include specific instructions or appoint a healthcare proxy to make decisions on their behalf, paralleling the role of the physicians in the Certification of Incapacity.
The Durable Power of Attorney for Healthcare is another important document that empowers a designated person to make medical decisions on behalf of someone who is incapacitated. Like the Certification of Incapacity, it focuses on the patient’s ability to understand and communicate their healthcare preferences. The Durable Power of Attorney provides a legal framework for someone trusted to act in the best interest of the patient, ensuring that their wishes are honored. Both documents emphasize the need for clarity in decision-making during critical health situations.
The Living Will is a specific type of Advance Directive that outlines an individual's preferences regarding end-of-life care. It is similar to the Certification of Incapacity in that it addresses situations where a person cannot express their wishes due to incapacity. Both documents aim to guide healthcare providers and loved ones in making decisions that reflect the patient's values and desires. The Living Will explicitly details the types of medical interventions a person does or does not want, providing a clear directive during difficult times.
The importance of having a proper legal document when purchasing a motorcycle cannot be overstated, as it provides both the buyer and seller with security during the transaction. A New York Motorcycle Bill of Sale form is crucial as it records all essential details about the sale, ensuring that both parties are protected. For more information on how to create or obtain this important document, you can visit autobillofsaleform.com/motorcycle-bill-of-sale-form/new-york-motorcycle-bill-of-sale-form/.
The Mental Health Advance Directive allows individuals to specify their preferences for mental health treatment in case they become unable to make decisions. This document shares similarities with the Certification of Incapacity, as both address situations where a person cannot communicate their choices. The Mental Health Advance Directive empowers individuals to outline their treatment preferences, ensuring that their mental health needs are respected and met, even when they cannot advocate for themselves.
The Physician Orders for Life-Sustaining Treatment (POLST) form is designed for individuals with serious health conditions who wish to specify their treatment preferences. Like the Certification of Incapacity, it focuses on the patient’s understanding of their medical situation and the implications of treatment options. The POLST form provides clear orders for healthcare providers, ensuring that the patient’s wishes are followed in emergencies. Both documents work together to ensure that medical decisions align with the patient’s values.
The Declaration for Mental Health Treatment is a legal document that allows individuals to express their treatment preferences in the event of a mental health crisis. Similar to the Certification of Incapacity, it is designed to guide healthcare providers in making decisions when a person cannot communicate their wishes. This declaration ensures that the individual’s preferences regarding medication and treatment are respected, paralleling the role of the physicians in assessing incapacity and guiding treatment decisions.
The Do Not Resuscitate (DNR) order is a medical order that indicates a person's wish not to receive cardiopulmonary resuscitation in the event of cardiac arrest. It shares similarities with the Certification of Incapacity by focusing on the patient's preferences regarding life-sustaining treatments. Both documents require clear communication of the individual’s wishes to healthcare providers, ensuring that their choices are honored in critical situations. The DNR order is a specific directive that complements the broader considerations outlined in the Certification of Incapacity.
The Healthcare Proxy form allows an individual to designate someone to make healthcare decisions on their behalf when they are unable to do so. This document is akin to the Certification of Incapacity, as both emphasize the importance of having someone trusted to advocate for the patient’s wishes. The Healthcare Proxy ensures that decisions align with the patient's values, much like the dual physician certifications in the Certification of Incapacity that confirm the patient's inability to make informed decisions.
Dos and Don'ts
When filling out the Certification Of Incapacity form, it’s important to follow certain guidelines to ensure accuracy and compliance. Here are five things you should and shouldn’t do:
- Do ensure that all fields are filled out completely and accurately.
- Do check the box for the appropriate evaluation of the patient's decision-making ability.
- Do sign and date the form immediately after the examination.
- Do keep a copy of the completed form for your records.
- Do review the patient’s medical history before making your assessment.
- Don’t leave any required fields blank, as this can delay the process.
- Don’t use vague language; be specific about the patient’s condition.
- Don’t forget to have a second physician examine the patient if required.
- Don’t make the certification more than two hours after the examination.
- Don’t rush through the form; take your time to ensure accuracy.
Key takeaways
Filling out the Certification of Incapacity form is a crucial process that ensures patients receive appropriate medical care when they cannot make informed decisions. Here are some key takeaways to consider:
- Two Physician Requirement: The form requires certification from two physicians. Each must independently assess the patient's ability to make informed medical decisions.
- Time Sensitivity: One of the certifications must be completed within two hours of the patient's examination. This time frame is essential to ensure the patient's current condition is accurately reflected.
- Clear Documentation: Physicians should provide detailed information about the patient's condition. This includes the nature of the incapacity and the specific medical treatments involved.
- Understanding Treatment: The form must indicate whether the patient is unable to understand the nature, extent, or probable consequences of the proposed treatment. This is a key factor in establishing incapacity.
- Communication Ability: Physicians must also check if the patient is unable to communicate a decision. This aspect is critical in determining the patient's capability to engage in informed consent.
- Legal Implications: The completed form serves as a legal document that can influence medical decisions and treatment plans. It is important to ensure accuracy and clarity in all entries.
How to Use Certification Of Incapacity
After completing the Certification of Incapacity form, the next steps involve ensuring that the form is signed by the appropriate medical professionals and submitted according to the specific requirements of your situation. This form must be filled out accurately to reflect the patient's current medical condition and their ability to make informed decisions regarding their treatment.
- Gather Necessary Information: Collect the patient's full name, date of birth, and details about their medical condition.
- Enter Physician Details: In the first section, write the name of the attending physician, including their title (M.D.), and fill in the date and time of the examination.
- Describe Patient's Condition: Clearly outline the patient's medical condition and specify the treatment in question. Be detailed but concise.
- Assess Patient's Decision-Making Ability: Indicate whether the patient is unable to evaluate the treatment options or communicate a decision by checking the appropriate box.
- Time Frame Certification: Confirm whether the attestation was made within two hours of the examination by checking the appropriate box.
- Sign and Date: The attending physician must sign and date the form, noting the time of the signature.
- Second Physician Certification: Repeat steps 2 through 6 for the second physician, ensuring all information is accurately filled out.
- Review the Completed Form: Check for any errors or missing information before submission to ensure compliance with requirements.