Printable Do Not Resuscitate Order Form
In the realm of healthcare, the Do Not Resuscitate (DNR) Order form serves as a crucial document that reflects an individual's wishes regarding end-of-life care. This form is designed for patients who, in the event of cardiac arrest or respiratory failure, prefer not to receive cardiopulmonary resuscitation (CPR) or other life-sustaining treatments. It is essential for patients to discuss their preferences with family members and healthcare providers to ensure that their wishes are clearly understood and respected. The DNR Order is typically signed by a physician and can be included in a patient’s medical record, making it easily accessible to medical personnel during emergencies. It is important to note that a DNR does not mean that a patient will receive no medical care; rather, it specifies the types of interventions that will not be performed. Understanding the implications of this form can empower individuals to make informed decisions about their healthcare and ensure that their values and preferences are honored at critical moments.
State-specific Tips for Do Not Resuscitate Order Templates
Common mistakes
-
Not discussing the decision with family or healthcare providers. Before filling out a Do Not Resuscitate (DNR) Order, it’s crucial to have conversations with loved ones and medical professionals. These discussions can clarify your wishes and ensure everyone understands your choices.
-
Failing to sign and date the form. A DNR Order must be signed and dated by the patient or their authorized representative. Without a signature, the document is not valid.
-
Using outdated forms. Ensure that you are using the most current version of the DNR Order form required by your state. Laws and regulations can change, and using an outdated form may lead to complications.
-
Not providing clear instructions. The form should clearly state your wishes regarding resuscitation. Vague language can lead to confusion and may not be honored in a medical emergency.
-
Neglecting to keep copies. After completing the DNR Order, make several copies. Share them with your healthcare providers, family members, and keep one in a visible place at home.
-
Overlooking state-specific requirements. Each state may have specific requirements for DNR Orders. Familiarize yourself with these to ensure your document complies with local laws.
-
Not updating the order when circumstances change. Life circumstances can change, such as a change in health status or personal beliefs. Regularly review and update your DNR Order as necessary.
-
Ignoring the need for witnesses or notarization. Some states require that the DNR Order be witnessed or notarized. Check your state’s regulations to avoid invalidating your wishes.
-
Forgetting to communicate your wishes to emergency personnel. Inform local emergency services about your DNR Order. This ensures they are aware of your wishes when responding to a medical emergency.
Preview - Do Not Resuscitate Order Form
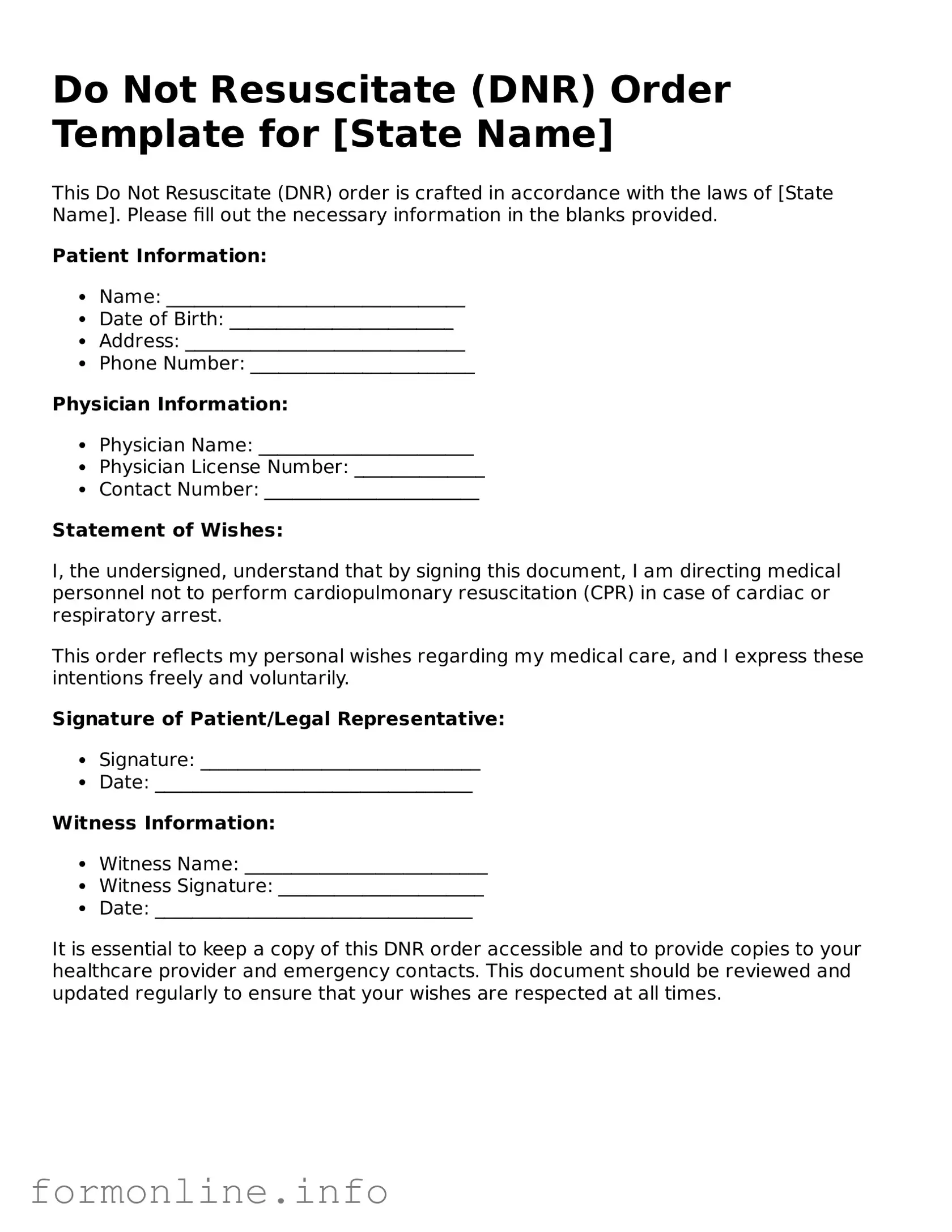
Do Not Resuscitate (DNR) Order Template for [State Name]
This Do Not Resuscitate (DNR) order is crafted in accordance with the laws of [State Name]. Please fill out the necessary information in the blanks provided.
Patient Information:
- Name: ________________________________
- Date of Birth: ________________________
- Address: ______________________________
- Phone Number: ________________________
Physician Information:
- Physician Name: _______________________
- Physician License Number: ______________
- Contact Number: _______________________
Statement of Wishes:
I, the undersigned, understand that by signing this document, I am directing medical personnel not to perform cardiopulmonary resuscitation (CPR) in case of cardiac or respiratory arrest.
This order reflects my personal wishes regarding my medical care, and I express these intentions freely and voluntarily.
Signature of Patient/Legal Representative:
- Signature: ______________________________
- Date: __________________________________
Witness Information:
- Witness Name: __________________________
- Witness Signature: ______________________
- Date: __________________________________
It is essential to keep a copy of this DNR order accessible and to provide copies to your healthcare provider and emergency contacts. This document should be reviewed and updated regularly to ensure that your wishes are respected at all times.
Common Forms:
I 751 Affidavit Sample - Affidavit letters must convey sincere personal thoughts, adding depth to the I-751 submission.
Personal Trainer Waiver Template - This document is key to a mutually respectful trainer-client interaction.
For those looking to understand their legal options, the informative guide on "Florida Power of Attorney forms" offers essential insights into the responsibilities and uses of this important document. You can find more details about how this form can help you at Power of Attorney in Florida.
Does Ca Dmv Power of Attorney Need to Be Notarized - Designate a representative who can legally manage your vehicle dealings when necessary.
Documents used along the form
A Do Not Resuscitate (DNR) Order is an important document that outlines a person's wishes regarding medical treatment in the event of a life-threatening situation. When considering a DNR, it's helpful to be aware of other related forms and documents that can provide additional clarity and support for healthcare decisions. Below is a list of documents often used alongside a DNR Order.
- Advance Healthcare Directive: This document allows individuals to specify their healthcare preferences in advance, including decisions about life-sustaining treatment and appointing a healthcare proxy.
- Living Will: A living will details an individual's wishes regarding medical treatment in situations where they are unable to communicate their preferences, particularly at the end of life.
- Healthcare Power of Attorney: This form designates a trusted person to make medical decisions on behalf of someone if they become incapacitated, ensuring that their wishes are honored.
- Physician Orders for Life-Sustaining Treatment (POLST): POLST is a medical order that translates a patient's wishes into actionable medical orders for emergency personnel, covering a range of treatment preferences.
- Do Not Intubate (DNI) Order: This document specifically instructs medical personnel not to insert a breathing tube in the event of respiratory failure, complementing a DNR Order.
- Trailer Bill of Sale: A key document for anyone buying or selling a trailer. It serves as proof of ownership and outlines essential details of the transaction, including the purchase price and trailer description. For more information, visit autobillofsaleform.com/trailer-bill-of-sale-form.
- Organ Donation Consent: This form allows individuals to express their wishes regarding organ donation after death, ensuring their intentions are known and respected.
- Medical Records Release Form: This document authorizes healthcare providers to share a person's medical records with designated individuals, which can be important for informed decision-making.
- Patient Information Form: This form collects essential information about a patient, including medical history and current medications, which can assist healthcare providers in emergencies.
- Emergency Contact List: This document includes names and contact information for individuals who should be reached in case of a medical emergency, ensuring that loved ones are informed and involved.
Understanding these documents can empower individuals and families to make informed decisions about medical care. Each form plays a unique role in ensuring that healthcare wishes are clearly communicated and respected, especially during critical moments.
Similar forms
A Living Will is a legal document that outlines a person’s wishes regarding medical treatment in the event they become unable to communicate their preferences. Like a Do Not Resuscitate (DNR) Order, it focuses on end-of-life care, specifying what types of medical interventions a person does or does not want. While a DNR specifically addresses resuscitation efforts, a Living Will can cover a broader range of medical decisions, providing guidance to healthcare providers and loved ones about the individual’s wishes.
A Healthcare Proxy, or Medical Power of Attorney, is another important document. It allows a person to designate someone else to make medical decisions on their behalf if they are unable to do so. Similar to a DNR, this document ensures that a person’s healthcare preferences are respected, especially in critical situations. While a DNR specifies what should not be done, a Healthcare Proxy empowers someone to make choices in line with the individual’s values and desires.
In addition to the various medical directives, individuals may also encounter legal documents related to property and ownership transactions, such as the Mobile Home Bill of Sale. This form is essential for clarifying the transfer of a mobile home, ensuring that all parties understand their rights and responsibilities during the transaction.
An Advance Directive combines elements of both a Living Will and a Healthcare Proxy. It serves as a comprehensive plan for medical care, detailing a person’s wishes regarding treatment options and appointing a trusted individual to make decisions. Like a DNR, it is designed to guide healthcare providers and family members during difficult times, ensuring that the person’s preferences are honored even if they cannot express them directly.
A Do Not Intubate (DNI) Order is another directive related to resuscitation efforts. It specifically indicates that a person does not want to be intubated if they experience respiratory failure. While a DNR focuses on cardiac arrest and resuscitation, a DNI addresses situations where breathing support may be necessary. Both documents are crucial for ensuring that a patient’s preferences regarding life-sustaining measures are respected.
A Comfort Care Order emphasizes the importance of palliative care and comfort in end-of-life situations. It guides healthcare providers to prioritize pain relief and quality of life over aggressive treatments. Similar to a DNR, it reflects the individual’s desire to avoid unnecessary interventions, focusing instead on providing comfort and dignity during the dying process.
A Medication Directive allows individuals to specify their preferences regarding medication use, particularly in end-of-life care. This document can complement a DNR by providing additional clarity on how medications should be managed. It ensures that healthcare providers understand the patient’s wishes regarding pain management and other treatments, aligning with their overall goals of care.
An Organ Donation Consent form is a separate but related document. While it does not directly address resuscitation, it reflects a person’s wishes regarding organ donation after death. Like a DNR, it is an important part of end-of-life planning, ensuring that an individual’s wishes regarding their body and legacy are respected in the event of their passing.
A Mental Health Advance Directive allows individuals to express their preferences for mental health treatment in case they become unable to make decisions. Similar to a DNR, it ensures that a person’s wishes are respected during a crisis. It can specify treatments they would or would not want, helping to guide caregivers and loved ones in difficult situations.
Lastly, a Family Caregiver Agreement can also be seen as a related document. It outlines the roles and responsibilities of family members or caregivers in managing a person’s care. While not a medical directive like a DNR, it ensures that everyone involved understands their role in respecting the individual’s wishes, particularly in situations where medical decisions may arise.
Dos and Don'ts
When filling out a Do Not Resuscitate (DNR) Order form, it's essential to approach the process with care. Here are ten important dos and don'ts to consider:
- Do ensure you fully understand the implications of a DNR order before signing.
- Do discuss your wishes with your healthcare provider and family members.
- Do keep the form in an accessible location, such as with your medical records.
- Do review and update your DNR order regularly as your health status changes.
- Do ask questions if you're unsure about any part of the form.
- Don't fill out the form under pressure or without sufficient information.
- Don't assume that verbal instructions are enough; always have a written DNR order.
- Don't forget to inform all relevant healthcare providers about your DNR order.
- Don't neglect to discuss your decision with loved ones to avoid confusion later.
- Don't leave the form unsigned or incomplete, as this may lead to unwanted resuscitation.
Key takeaways
When filling out and using a Do Not Resuscitate (DNR) Order form, it is important to understand its purpose and implications. Here are some key takeaways:
- Understand the Purpose: A DNR order is a legal document that indicates a person's wishes regarding resuscitation efforts in the event of a medical emergency.
- Consult with Healthcare Providers: Before completing the form, it is advisable to discuss your wishes with healthcare professionals. They can provide valuable insights and guidance.
- Ensure Proper Documentation: After filling out the DNR order, make sure it is signed and dated. Keep copies accessible to family members and healthcare providers.
- Review Regularly: As circumstances and health conditions change, it is important to review and update the DNR order as needed to reflect current wishes.
How to Use Do Not Resuscitate Order
Filling out a Do Not Resuscitate Order form is an important step in ensuring your healthcare wishes are respected. Once you have completed the form, it should be shared with your healthcare provider and kept in a place where it can be easily accessed in case of an emergency.
- Obtain the Do Not Resuscitate Order form from your healthcare provider or download it from a reliable source.
- Read the instructions carefully to understand the requirements of the form.
- Fill in your full name, date of birth, and any other personal information requested at the top of the form.
- Indicate your wishes regarding resuscitation by checking the appropriate box or writing your preference in the designated area.
- Provide the name and contact information of your healthcare provider, if required.
- Sign and date the form to validate your wishes.
- Have a witness sign the form, if necessary, according to your state’s requirements.
- Make copies of the completed form for your records and for your healthcare provider.
- Discuss your decision with your family and healthcare team to ensure everyone is aware of your wishes.