Fill Out a Valid Medication Administration Record Sheet Form
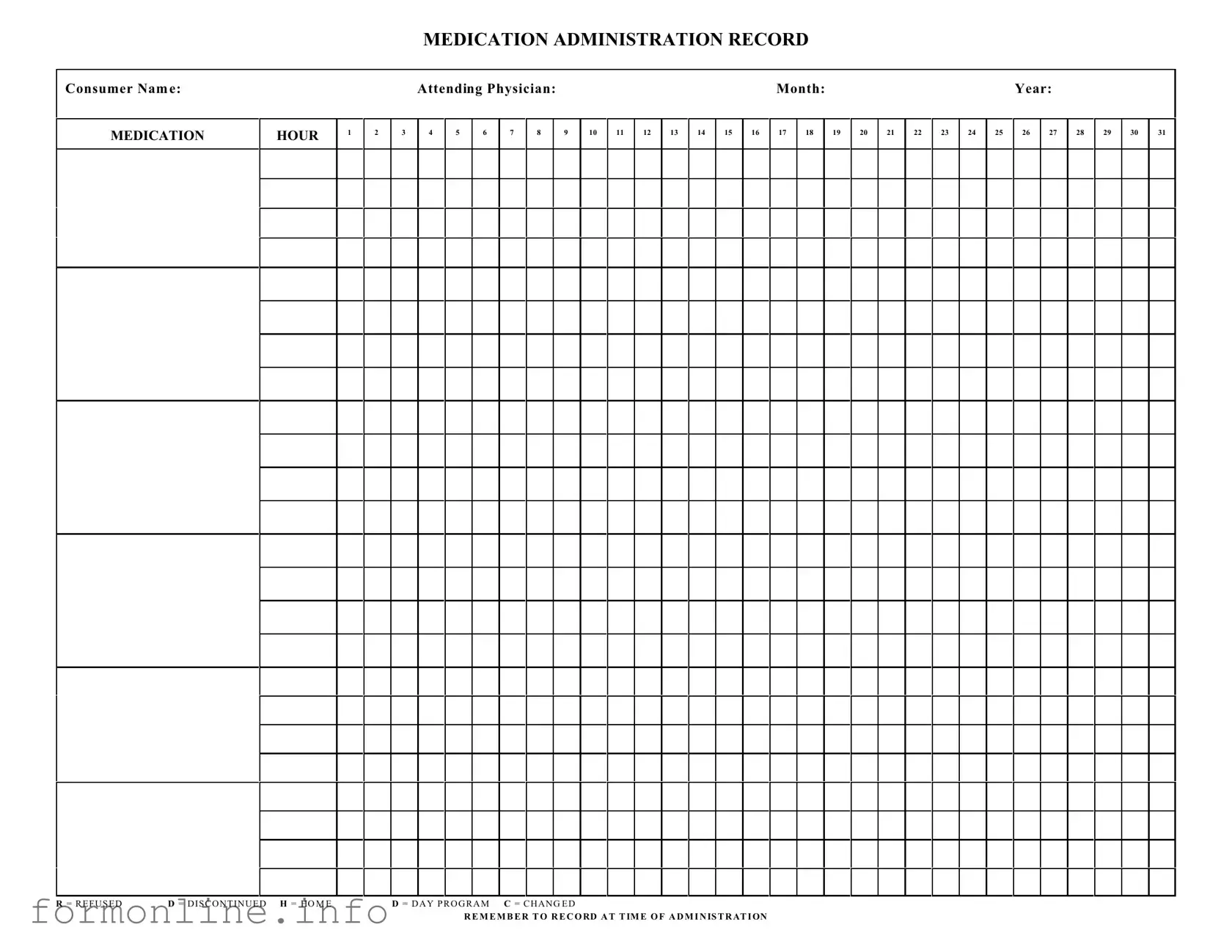
The Medication Administration Record Sheet (MARS) serves as a crucial tool in the healthcare landscape, particularly in ensuring the safe and effective administration of medications to patients. This form captures essential information such as the consumer's name, the attending physician's details, and the specific month and year of medication administration. Each hour of the day is meticulously documented, allowing healthcare providers to track when medications are given. The form includes a comprehensive grid where healthcare professionals can record various statuses, including whether a medication was refused, discontinued, or changed. Such meticulous documentation is not merely a formality; it is a safeguard that promotes accountability and transparency in patient care. By recording the administration time accurately, providers can ensure that patients receive their medications as prescribed, thereby minimizing the risk of errors and enhancing overall treatment outcomes. Understanding the significance of the MARS is imperative for anyone involved in patient care, as it underpins the very foundation of medication management and patient safety.
Common mistakes
-
Inaccurate Consumer Information: One of the most common mistakes is failing to accurately fill in the consumer's name. This can lead to confusion and errors in medication administration.
-
Missing Attending Physician's Name: Omitting the name of the attending physician can complicate communication and accountability, especially in emergencies.
-
Incorrect Date or Month: Entering the wrong month or year can create significant issues in tracking medication history. Always double-check these entries.
-
Failure to Record Administration Times: It's crucial to record the time of administration. Missing this information can lead to improper dosing schedules.
-
Neglecting to Use Correct Abbreviations: Using incorrect abbreviations for refused or discontinued medications can lead to misunderstandings. Familiarize yourself with the standard abbreviations.
-
Not Documenting Changes: If there are any changes in medication, failing to document them can result in serious health risks. Ensure that all changes are recorded promptly and accurately.
Preview - Medication Administration Record Sheet Form
MEDICATION ADMINISTRATION RECORD
Consumer Nam e:
MEDICATION
HOUR
1
2
|
Attending Physician: |
|
|
|
|
|
|
|
|
Month: |
|
|
|
|
|
|
|
Year: |
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3 |
4 |
5 |
6 |
7 |
8 |
|
9 |
10 |
11 |
12 |
13 |
14 |
15 |
16 |
17 |
18 |
|
19 |
20 |
21 |
22 |
23 |
24 |
25 |
26 |
27 |
28 |
29 |
30 |
31 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
R = R E F U S E D |
D = D I S C O N T I N U E D H = HO M E |
D = D A Y P R O G R A M C = C H A N G E D |
R E M E M B E R T O R E C O RD A T T IM E O F A D M I N IS T R AT I ON
Other PDF Templates
What Is Recorded on a Medicine Label Uk - Contains any relevant studies or trials associated with the medication.
The Washington Mobile Home Bill of Sale form is crucial for anyone looking to transfer ownership of a mobile home. This legal document not only details the buyer's and seller's information but also includes the mobile home's description and the agreed sale price. For those interested, a comprehensive guide can be found at the Mobile Home Bill of Sale, ensuring that all aspects of the transaction are clearly outlined and legally binding, thus protecting both parties involved.
3613a - Each incident category is clearly defined for accurate reporting of events.
Documents used along the form
The Medication Administration Record Sheet is an essential document used in healthcare settings to track the administration of medications to patients. Alongside this form, several other documents play a crucial role in ensuring accurate medication management and patient safety. Below is a list of related forms and documents that are commonly utilized in conjunction with the Medication Administration Record Sheet.
- Medication Order Form: This form provides detailed instructions from a physician regarding the medications prescribed to a patient, including dosage, frequency, and route of administration.
- Patient Medication History: This document compiles a patient's previous and current medications, helping healthcare providers understand potential interactions and allergies.
- Medication Reconciliation Form: Used during transitions of care, this form ensures that a patient's medication list is accurate and complete, reducing the risk of errors.
- Adverse Drug Reaction Report: This form is completed when a patient experiences negative side effects from a medication, documenting the incident for further review and analysis.
- Patient Consent Form: Before administering certain medications, especially those with significant risks, this form confirms that the patient has been informed and consents to the treatment.
- Medication Administration Policy: This document outlines the procedures and protocols for administering medications within a healthcare facility, ensuring compliance with regulations.
- Pharmacy Communication Log: This log facilitates communication between nursing staff and pharmacy, documenting any medication-related inquiries or issues that arise.
- Incident Report Form: If a medication error occurs, this form captures details about the incident, which is essential for quality improvement and preventing future occurrences.
- Patient Education Materials: These resources provide information to patients about their medications, including how to take them and what side effects to watch for.
- Arizona RV Bill of Sale Form: A formal document essential for the transfer of ownership of a recreational vehicle, ensuring protection and legality for both parties involved in the transaction. More information can be found at https://autobillofsaleform.com/rv-bill-of-sale-form/arizona-rv-bill-of-sale-form.
- Daily Progress Notes: Healthcare providers use these notes to document a patient's condition and response to medications, which is vital for ongoing care management.
Each of these documents plays a significant role in the overall medication management process, helping to ensure that patients receive safe and effective care. Proper documentation and communication among healthcare providers are key components in minimizing errors and enhancing patient outcomes.
Similar forms
The Medication Administration Record (MAR) is similar to the Patient Care Plan. Both documents serve as essential tools for healthcare providers to ensure that patients receive appropriate treatment. The Patient Care Plan outlines the goals, interventions, and expected outcomes for a patient’s care, while the MAR specifically tracks the administration of medications. Together, they create a comprehensive overview of a patient’s treatment, allowing for better coordination among healthcare professionals and ensuring that all aspects of a patient’s care are addressed effectively.
Another document that resembles the MAR is the Nursing Progress Notes. These notes provide a chronological account of a patient’s condition and response to treatment, including medication administration. While the MAR focuses solely on the timing and specifics of medication given, Nursing Progress Notes offer a broader context by detailing observations, assessments, and any changes in the patient’s condition. This synergy allows for a more holistic understanding of the patient's journey through care.
The Florida Motor Vehicle Power of Attorney form is an important document for those needing to delegate vehicle-related responsibilities. It allows individuals to appoint someone else to act on their behalf in transactions involving motor vehicles. For more detailed information, the comprehensive Florida Motor Vehicle Power of Attorney form can be found at the official site.
Additionally, the Treatment Administration Record (TAR) can be compared to the MAR. The TAR is used primarily in settings where various treatments, not just medications, are administered. It records the administration of therapies such as injections, wound care, or other interventions. While the MAR is specifically dedicated to medications, both documents are vital for ensuring that patients receive the correct treatment at the right time, thus enhancing overall patient safety and care quality.
Lastly, the Consent for Treatment Form bears a resemblance to the MAR in that it documents patient consent for specific medical interventions, including medication administration. While the MAR tracks what medications have been given, the Consent for Treatment Form ensures that patients are informed and agree to their treatment plans. This document is crucial for respecting patient autonomy and legal requirements in healthcare, reinforcing the importance of communication and trust in the patient-provider relationship.
Dos and Don'ts
When filling out the Medication Administration Record Sheet, it’s essential to follow specific guidelines to ensure accuracy and compliance. Here’s a list of things you should and shouldn’t do:
- Do ensure that the consumer's name is clearly written at the top of the form.
- Do accurately record the medication administration time for each dose.
- Do use the correct codes (R, D, H, M, C) to indicate the status of the medication.
- Do double-check the dosage and medication name before filling out the record.
- Don't leave any fields blank; every section should be completed appropriately.
- Don't use abbreviations that are not standard or widely recognized.
- Don't alter the record after it has been filled out; any changes should be documented separately.
Key takeaways
Filling out and utilizing the Medication Administration Record Sheet form is crucial for ensuring accurate medication management. Here are some key takeaways to keep in mind:
- Complete Consumer Information: Always start by filling in the consumer's name clearly at the top of the form.
- Document the Attending Physician: Include the name of the attending physician to maintain a clear chain of responsibility.
- Specify the Month and Year: Clearly indicate the month and year for which the medications are being administered.
- Record Medication Administration Times: Use the designated hours to document when each medication is given.
- Indicate Refusals and Changes: Use the provided codes (R, D, H, C) to accurately reflect any refusals, discontinuations, or changes in medication.
- Maintain Consistency: Ensure that the same format is used throughout the form to avoid confusion.
- Timely Recording: Always record information at the time of administration to ensure accuracy and reliability.
- Monitor for Errors: Regularly check the form for any potential errors or omissions that may arise.
- Review Regularly: Conduct periodic reviews of the Medication Administration Record Sheet to ensure compliance with medication protocols.
- Communicate with the Healthcare Team: Share the completed form with the healthcare team to ensure everyone is informed about the consumer’s medication status.
By following these guidelines, you can help ensure that medication administration is carried out safely and effectively.
How to Use Medication Administration Record Sheet
Filling out the Medication Administration Record Sheet is a straightforward process that ensures accurate documentation of medication administration. Proper completion of this form is essential for maintaining a clear record of the medications given to a consumer, which can be critical for their health management.
- Begin by entering the Consumer Name at the top of the form.
- Next, fill in the Attending Physician name to indicate who is responsible for the consumer's care.
- Record the Month and Year in the designated spaces to specify the time frame for the medication records.
- In the column labeled MEDICATION, list each medication that the consumer is prescribed.
- For each medication, mark the appropriate HOUR columns (1 through 31) to indicate when the medication is administered.
- If a medication was refused, use R to denote this in the corresponding hour column.
- In case a medication is discontinued, mark it with D.
- If the consumer is at home, indicate this with H.
- For medications given during a day program, use D P.
- If there are any changes in medication, mark this with C.
- Finally, remember to record the time of administration accurately in the respective hour columns.