Fill Out a Valid Medication Count Sheet Form
The Medication Count Sheet form plays a crucial role in ensuring the accurate tracking of medications administered to residents in various care settings. This form typically includes essential details such as the resident's name, the quantity of medication on hand, and the date the medication was started. It also captures the drug's strength, which is vital for proper dosing. Staff members are required to sign the sheet, providing accountability for the administration of medication. Additionally, the form records the time and quantity of medication administered, along with the remaining amount after administration. By maintaining this documentation, facilities can enhance safety and compliance in medication management, ultimately supporting the well-being of residents.
Common mistakes
-
Failing to include the resident's name at the top of the form. This can lead to confusion about whose medication is being counted.
-
Not recording the date started for each medication. This information is crucial for tracking treatment timelines.
-
Omitting the drug strength of the medication. Without this detail, it becomes difficult to ensure the correct dosage is administered.
-
Using inconsistent quantity measurements. Ensure that all quantities are recorded in the same unit (e.g., milligrams, milliliters) to avoid errors.
-
Forgetting to sign the staff signature section. This is essential for accountability and tracking who administered the medication.
-
Neglecting to fill in the date and time when medication is administered. This information helps maintain an accurate medication schedule.
-
Not updating the quantity on hand after administration. This can lead to discrepancies in medication counts.
-
Failing to record the remaining quantity accurately. This is vital for monitoring medication inventory and ensuring availability.
-
Leaving the form incomplete or partially filled. All sections should be filled out to maintain clarity and compliance.
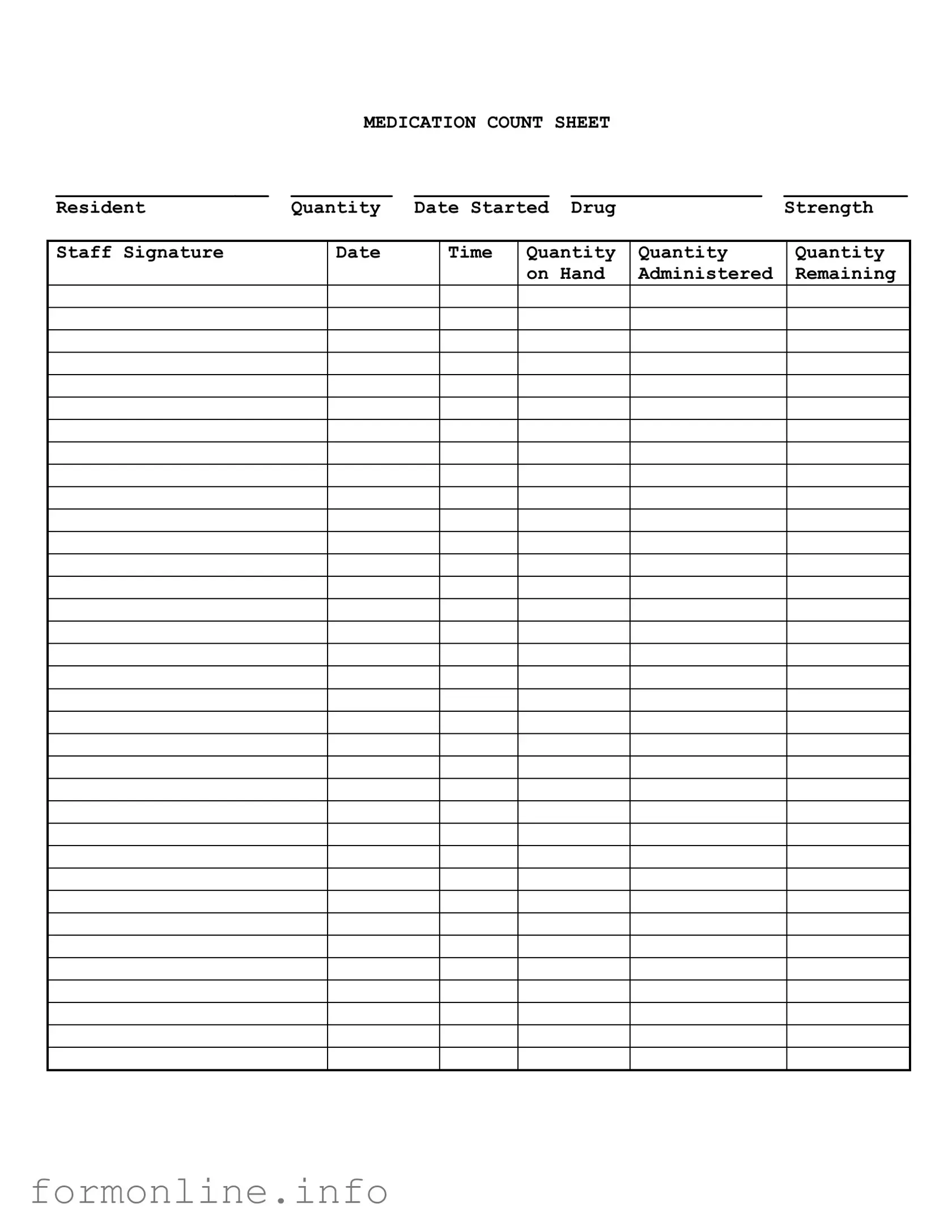
Preview - Medication Count Sheet Form
|
MEDICATION COUNT SHEET |
|
||
___________________ |
_________ |
____________ |
_________________ |
___________ |
Resident |
Quantity |
Date Started |
Drug |
Strength |
Staff Signature
Date
Time
Quantity |
Quantity |
Quantity |
on Hand |
Administered |
Remaining |
|
|
|
Other PDF Templates
Futa Wages - Understanding the intricacies of Form 940 can enhance an employer's tax strategy.
When engaging in the sale or transfer of a mobile home in Connecticut, it is essential to utilize the Connecticut Mobile Home Bill of Sale form, which serves as a fundamental legal document to clarify ownership changes and secure both parties' interests. This form includes key details such as the names of the buyer and seller, the identification information of the mobile home, and the agreed purchase price, ensuring that all aspects of the transaction are transparent and legally binding. For more information, you can refer to the Mobile Home Bill of Sale.
Form I-134 Affidavit of Support - Different visa categories may have different requirements regarding the I-134.
Da Form 1380 May 2019 - The scope of the form can range across different duty types, requiring careful documentation.
Documents used along the form
The Medication Count Sheet is an essential tool used in healthcare settings to track the administration and inventory of medications. Alongside this form, several other documents are commonly utilized to ensure proper medication management and patient safety. Below are five forms that complement the Medication Count Sheet, each serving a specific purpose in the medication administration process.
- Medication Administration Record (MAR): This document provides a detailed log of each medication administered to a resident. It includes the name of the medication, dosage, route, and time of administration. The MAR is crucial for ensuring that patients receive their medications as prescribed.
- Prescription Order: A prescription order is a formal document written by a healthcare provider that authorizes a patient to receive a specific medication. It includes details such as the patient's name, medication name, dosage, and instructions for use. This document is vital for legal and clinical purposes.
- Tennessee Homeschool Letter of Intent: This formal document is essential for notifying the local school district of a family's decision to homeschool, ensuring compliance with state regulations. For more information, see the Homeschool Letter of Intent.
- Medication Reconciliation Form: This form is used to compare a patient's current medications with those prescribed during a healthcare visit or hospital admission. It helps identify any discrepancies and ensures continuity of care, reducing the risk of medication errors.
- Incident Report: If a medication error occurs, an incident report is filled out to document the event. This form captures details about what happened, the individuals involved, and any actions taken in response. It is essential for quality assurance and improving safety protocols.
- Patient Education Materials: These are informational documents provided to patients regarding their medications. They often include instructions on how to take the medication, potential side effects, and important safety information. Educating patients empowers them to manage their health effectively.
Incorporating these documents alongside the Medication Count Sheet enhances the overall medication management process. Each form plays a crucial role in ensuring that medications are administered safely and effectively, ultimately contributing to better patient outcomes.
Similar forms
The Medication Administration Record (MAR) is a critical document used in healthcare settings. Like the Medication Count Sheet, the MAR tracks the administration of medications to patients. It includes details such as the resident's name, the drug name, dosage, and the times medications are given. Both forms require staff signatures to confirm that medications have been administered correctly, ensuring accountability and accuracy in medication management.
The Patient Medication Profile serves a similar purpose by providing a comprehensive overview of a patient's medication history. This document lists all medications prescribed to a patient, including dosages and administration schedules. While the Medication Count Sheet focuses on the quantity of medications on hand, the Patient Medication Profile emphasizes the patient's ongoing treatment plan, making it essential for continuity of care.
Understanding the significance of a Durable Power of Attorney form in Florida can be pivotal for individuals planning their financial and legal responsibilities. This form not only grants authority to another individual for decision-making but also ensures that your preferences are honored during challenging times.
The Prescription Order form is another document that shares similarities with the Medication Count Sheet. This form is used to communicate medication orders from healthcare providers to pharmacies. It includes information such as the drug name, dosage, and instructions for use. Both documents aim to ensure that the correct medications are available and administered to patients, though the Prescription Order is more focused on the initial ordering process.
The Inventory Control Sheet is vital for managing medication supplies within a facility. Similar to the Medication Count Sheet, it tracks the quantities of medications on hand. This document helps staff monitor stock levels and reorder medications as needed. Both forms play a role in preventing medication shortages and ensuring that the necessary drugs are available for patient care.
The Incident Report form is used to document any medication errors or adverse drug reactions. While the Medication Count Sheet focuses on tracking medication quantities, the Incident Report captures information about what went wrong during medication administration. Both documents are essential for improving patient safety and quality of care, as they help identify areas for improvement in medication management practices.
The Medication Reconciliation form is used during transitions of care, such as hospital admissions or discharges. It compares a patient's current medications with those prescribed during their stay. Like the Medication Count Sheet, it ensures that patients receive the correct medications, but it emphasizes the importance of accurate medication lists to prevent errors during transitions.
The Controlled Substance Log is specifically designed to track the use of controlled substances within a facility. It shares similarities with the Medication Count Sheet in that it requires careful documentation of quantities on hand and administered. Both forms are essential for compliance with regulatory requirements and for maintaining accurate records of medication usage.
The Treatment Administration Record (TAR) is used to document non-medication treatments provided to patients. While it differs in focus, the TAR shares the same goal of ensuring accurate record-keeping and accountability among staff. Both the TAR and the Medication Count Sheet require staff signatures to confirm that treatments or medications have been administered as prescribed.
The Medication Error Reporting form is crucial for documenting any mistakes made during medication administration. This form is similar to the Medication Count Sheet in that it aims to improve patient safety. While the Count Sheet tracks quantities, the Error Reporting form analyzes the causes of errors to prevent future occurrences, highlighting the importance of thorough documentation in medication management.
The Daily Medication Log is a straightforward record that tracks daily medication administration for each resident. Like the Medication Count Sheet, it includes essential details such as drug names and quantities administered. Both documents are designed to provide clear and accurate records to support effective medication management and ensure that patients receive their prescribed treatments on time.
Dos and Don'ts
When filling out the Medication Count Sheet form, attention to detail is crucial. Here are some important dos and don’ts to keep in mind:
- Do ensure all sections of the form are completed, including resident name, drug strength, and quantity.
- Do double-check the quantities recorded to avoid discrepancies.
- Do sign and date the form after each entry to maintain accountability.
- Do record the time of administration accurately to track medication schedules.
- Don’t leave any fields blank; incomplete forms can lead to confusion.
- Don’t use correction fluid or erase entries; instead, draw a line through mistakes and initial them.
- Don’t forget to update the remaining quantity after each administration to ensure accurate counts.
Key takeaways
When filling out and using the Medication Count Sheet form, it is essential to follow certain guidelines to ensure accuracy and compliance. Here are some key takeaways to consider:
- Accuracy is Crucial: Always double-check the information entered on the form. Errors in dosage or medication can lead to serious health risks.
- Document Everything: Record the date, time, and quantity of medication administered. This documentation is vital for tracking and accountability.
- Use Clear Signatures: Ensure that staff signatures are legible. Clear identification of who administered the medication is important for transparency.
- Regular Updates: Update the quantity on hand after each administration. Keeping this information current helps prevent discrepancies.
- Monitor Drug Strength: Pay attention to the drug strength listed on the form. This ensures that the correct dosage is being administered.
- Review Periodically: Regularly review the Medication Count Sheet to identify any patterns or issues that may need addressing. This proactive approach can enhance patient safety.
How to Use Medication Count Sheet
Filling out the Medication Count Sheet is an important task that ensures accurate tracking of medications. Follow these steps carefully to complete the form correctly.
- Start by writing the resident's name at the top of the sheet.
- Fill in the quantity of medication available at the beginning of the count.
- Enter the date the medication was started in the designated space.
- List the drug name in the appropriate section.
- Specify the drug strength as indicated on the medication packaging.
- Sign the form in the staff signature area to confirm the count.
- Record the date and time of the count in the provided fields.
- Document the quantity administered during the count period.
- Calculate and write down the remaining quantity of medication on hand.