Fill Out a Valid Progress Notes Form
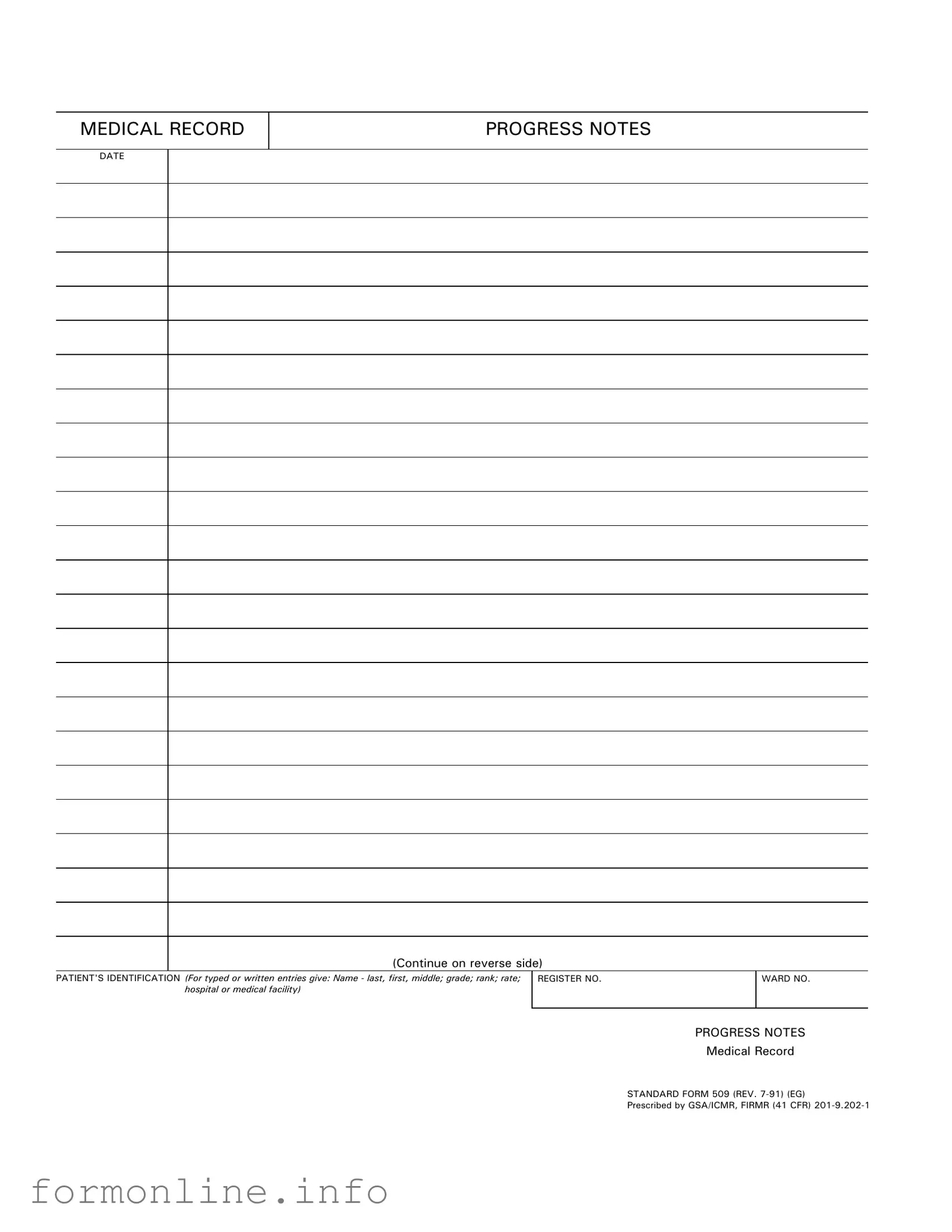
The Progress Notes form plays a crucial role in the documentation of patient care, serving as a vital tool for healthcare professionals. This standardized form, identified as Medical Record Standard Form 509, is designed to capture essential information about a patient’s treatment and progress over time. It includes key details such as the date of the entry, the patient's identification information—comprising their name, grade, rank, and hospital or medical facility—along with their registration and ward numbers. By maintaining a consistent format, the Progress Notes form ensures that all relevant data is easily accessible and organized, facilitating effective communication among medical staff. The form is not only a record of events but also a means to evaluate the effectiveness of treatment plans and make necessary adjustments. Ultimately, the Progress Notes are indispensable for providing quality care and ensuring continuity in a patient's medical journey.
Common mistakes
-
Incomplete Patient Identification: Failing to provide the full name, grade, rank, or rate of the patient can lead to confusion and miscommunication. Ensure all fields are filled out completely.
-
Incorrect Date Entry: Entering the wrong date can create discrepancies in the medical record. Always double-check the date to ensure accuracy.
-
Neglecting to Use Standard Terminology: Using non-standard terms or abbreviations may result in misunderstandings. Stick to commonly accepted medical language to maintain clarity.
-
Omitting Important Details: Leaving out significant observations or changes in the patient's condition can hinder proper treatment. Document all relevant information thoroughly.
-
Not Following the Correct Format: Failing to adhere to the prescribed format of the Progress Notes can lead to disorganization. Always follow the layout specified in the Standard Form 509.
Preview - Progress Notes Form
MEDICAL RECORD
PROGRESS NOTES
DATE
(Continue on reverse side)
PATIENT'S IDENTIFICATION (For typed or written entries give: Name - last, first, middle; grade; rank; rate; hospital or medical facility)
REGISTER NO. |
WARD NO. |
|
|
PROGRESS NOTES
Medical Record
STANDARD FORM 509 (REV.
Prescribed by GSA/ICMR, FIRMR (41 CFR)
PROGRESS NOTES
DATE
STANDARD FORM 509 (REV.
Other PDF Templates
Dd 2656 March 2022 - Completing the DD 2656 can affect future financial entitlements.
In order to properly navigate the filing process and ensure compliance, employers can seek additional information and guidance regarding the WC-1 Georgia form at georgiapdf.com/, which provides valuable resources and assistance for timely submissions.
Florida Immunization Registry - This form is essential for school entry and attendance in Florida.
Documents used along the form
The Progress Notes form is a vital component of a patient's medical record, documenting their ongoing care and treatment. Alongside this form, several other documents are frequently used to ensure comprehensive patient management and communication among healthcare providers. Below is a list of these documents, each serving a specific purpose.
- Admission Assessment Form: This document is completed upon a patient's entry into a healthcare facility. It gathers essential information about the patient's medical history, current health status, and any immediate needs for care.
- Care Plan: A care plan outlines the patient's treatment goals and strategies. It is developed collaboratively by healthcare providers and the patient, ensuring that everyone is aligned on the expected outcomes and interventions.
- Medication Administration Record (MAR): The MAR tracks all medications administered to the patient during their stay. It includes details such as dosages, times of administration, and any reactions noted, ensuring safe and accurate medication management.
- Discharge Summary: This document is prepared when a patient is ready to leave the healthcare facility. It summarizes the patient's treatment, progress, and any follow-up care or instructions needed post-discharge.
- Referral Form: When a patient requires specialized care, a referral form is used to communicate their needs to another healthcare provider. This document includes relevant medical history and the reason for the referral.
- RV Bill of Sale: For those transferring ownership of a recreational vehicle in Arizona, it's essential to complete an RV Bill of Sale. This legal document, which can be found at https://autobillofsaleform.com/rv-bill-of-sale-form/arizona-rv-bill-of-sale-form/, serves as proof of purchase and details the transaction between the seller and buyer, safeguarding both parties involved in the sale.
- Incident Report: If any unusual events occur during a patient's care, an incident report is filed. This document captures details about the event, the individuals involved, and any actions taken in response, promoting safety and accountability.
- Patient Consent Form: Before any treatment or procedure, a patient must provide informed consent. This form outlines the risks, benefits, and alternatives to the proposed care, ensuring that the patient understands and agrees to the treatment plan.
These documents, along with the Progress Notes form, create a comprehensive picture of a patient's care journey. Each serves a critical role in maintaining accurate and effective communication among healthcare professionals, ultimately supporting better patient outcomes.
Similar forms
The Treatment Plan is similar to the Progress Notes form as it documents the patient’s care strategy. It outlines the goals, interventions, and expected outcomes for the patient. Like Progress Notes, it is an essential part of the medical record, ensuring that all healthcare providers involved are aligned on the patient’s treatment. Both documents serve to track the patient's journey and facilitate communication among the care team.
In the realm of mobile home transactions, it is essential to utilize proper documentation to facilitate a legal transfer of ownership. One crucial document that helps avoid any ambiguities during this process is the Mobile Home Bill of Sale, which details important information about the buyer, seller, and the mobile home being sold. Ensuring that this form is accurately filled out and maintained helps protect the rights of both parties involved in the sale.
The SOAP Notes format, which stands for Subjective, Objective, Assessment, and Plan, shares similarities with Progress Notes. SOAP Notes provide a structured way to document patient encounters. They capture the patient’s reported symptoms, clinical findings, assessments, and plans for treatment. This methodical approach helps in maintaining clarity and continuity of care, much like the Progress Notes.
Discharge Summaries are another document that aligns closely with Progress Notes. Discharge Summaries provide a comprehensive overview of a patient's hospital stay, including treatments received and follow-up care instructions. Both documents emphasize the importance of continuity in care and provide critical information for future healthcare providers.
Clinical Summaries also resemble Progress Notes in their purpose of conveying essential patient information. These summaries often include a brief history, treatment details, and follow-up recommendations. They serve as a quick reference for healthcare providers and ensure that critical information is readily available, similar to how Progress Notes function.
Patient Care Plans are akin to Progress Notes as they detail the specific interventions and strategies for managing a patient's care. These plans include goals and objectives tailored to the patient’s needs. Both documents are crucial for ensuring that all team members are informed and that care is coordinated effectively.
Medication Administration Records (MAR) share a connection with Progress Notes by documenting the medications given to a patient. MARs track dosages, times, and any reactions or side effects. This record-keeping is vital for patient safety and helps healthcare providers monitor the effectiveness of treatments, just as Progress Notes do.
Referral Forms also have similarities with Progress Notes. They provide essential information about a patient’s condition and the reason for referral to another specialist. Both documents facilitate communication among healthcare providers, ensuring that the receiving provider has a clear understanding of the patient’s history and needs.
Encounter Forms are another document that parallels Progress Notes. These forms capture information about the services provided during a patient visit, including diagnoses and procedures performed. Like Progress Notes, they play a critical role in documenting patient interactions and ensuring accurate billing and coding.
Health Risk Assessments (HRAs) are similar to Progress Notes in that they evaluate a patient’s health status and potential risks. HRAs often include lifestyle information and medical history, helping healthcare providers develop a comprehensive understanding of the patient. Both documents aim to inform treatment decisions and improve patient outcomes.
Finally, Case Management Notes reflect similarities with Progress Notes by documenting ongoing patient assessments and care coordination efforts. These notes track the progress of a patient’s treatment plan and any barriers to care. Both documents are essential for ensuring that patients receive the appropriate resources and support throughout their healthcare journey.
Dos and Don'ts
When filling out the Progress Notes form, there are important practices to follow to ensure accuracy and compliance. Here are five key dos and don'ts:
- Do include the patient's full name, grade, rank, and rate in the identification section.
- Do ensure that the date is clearly indicated on the form.
- Do write legibly, whether typing or handwriting the entries.
- Do use clear and concise language when documenting progress notes.
- Do review the completed form for any errors before submission.
- Don't leave out any required identification information.
- Don't use abbreviations that may not be universally understood.
- Don't write in a way that could be misinterpreted; clarity is essential.
- Don't forget to sign and date the form if required.
- Don't submit the form without checking for completeness.
Key takeaways
When it comes to filling out and using the Progress Notes form, there are several important considerations to keep in mind. Here are five key takeaways to ensure accurate and effective documentation:
- Accuracy is crucial. Always provide the patient's full name, including last, first, and middle names, along with their grade, rank, and rate. This helps maintain clear and organized records.
- Include identification details. Make sure to fill in the patient’s identification number and the ward number. This information is essential for proper tracking and retrieval of medical records.
- Document timely. Record progress notes as soon as possible after patient interactions. Timely documentation enhances the quality of care and ensures that all relevant information is captured accurately.
- Use clear language. Write in a straightforward manner. Avoid using abbreviations or jargon that may not be understood by all members of the healthcare team.
- Follow standard procedures. Adhere to the guidelines outlined for the Progress Notes form, including the use of the correct version of the form, to ensure compliance with medical record standards.
How to Use Progress Notes
After gathering the necessary information, you can begin filling out the Progress Notes form. This process involves providing specific details about the patient and the medical encounter. Follow these steps carefully to ensure accurate and complete documentation.
- Date: Write the date of the medical encounter at the top of the form.
- Patient's Identification: Fill in the patient's name (last, first, middle), grade, rank, rate, and the name of the hospital or medical facility.
- Register No: Enter the patient's register number.
- Ward No: Indicate the ward number where the patient is located.
- Progress Notes: Provide detailed notes regarding the patient's condition, treatment, and any other relevant information.
Once you have completed the form, review it for accuracy. Make sure all information is clear and legible before submitting it as part of the medical record.