Fill Out a Valid Tb Test Form
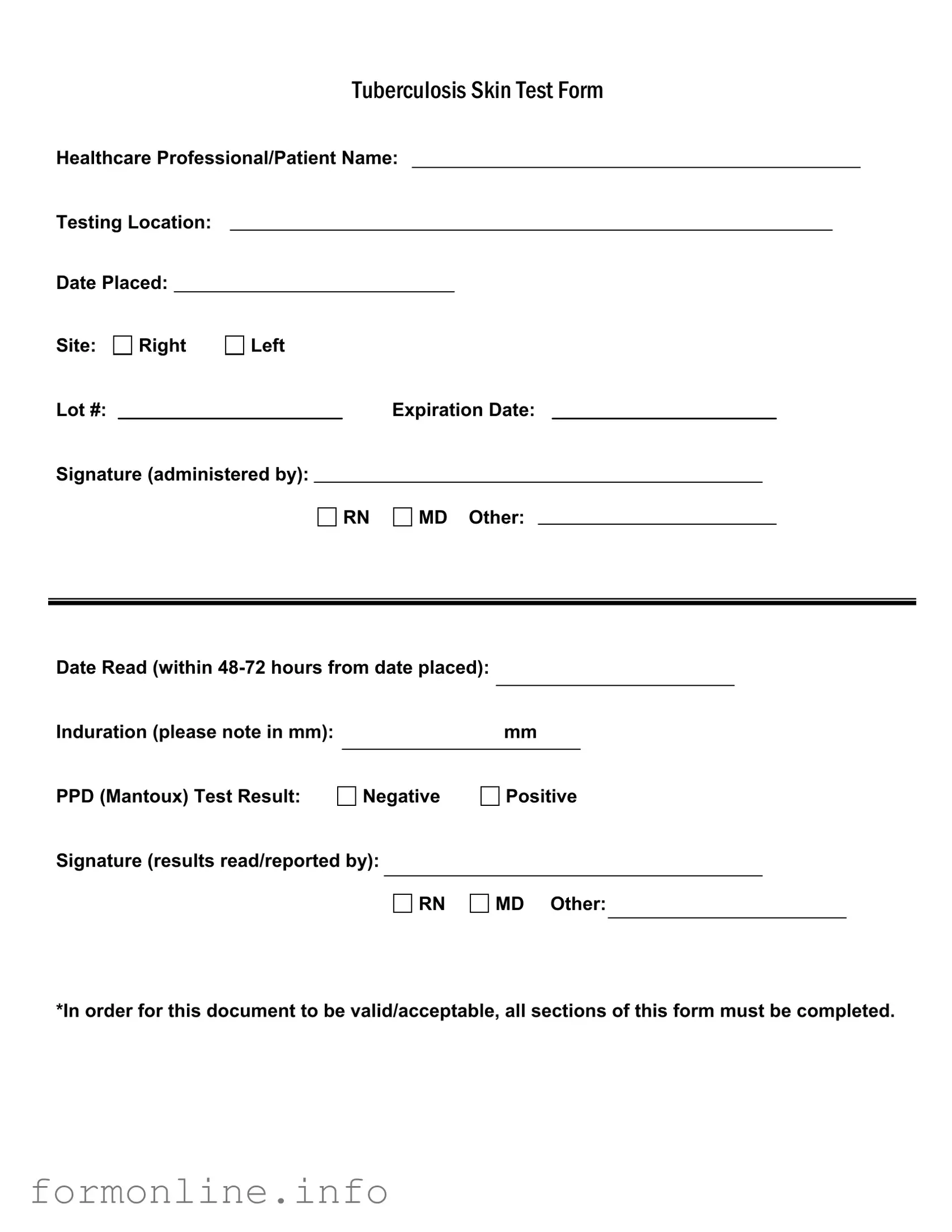
The Tuberculosis (TB) Skin Test Form is a crucial document used in the assessment and monitoring of tuberculosis exposure. This form captures essential information, including the names of both the healthcare professional and the patient, as well as the location where the test is administered. It outlines critical details such as the date the test was placed, the site of administration, and the specific lot number along with its expiration date. The signature of the administering professional—whether an RN, MD, or another qualified individual—is also required to validate the procedure. Furthermore, the form must be completed with the date the test is read, which must occur within 48 to 72 hours from placement. It includes a measurement of induration, noted in millimeters, to determine the test's result, which can be either negative or positive. The form concludes with a second signature from the professional who reads and reports the results. To ensure its validity, every section of this form must be filled out accurately and completely, underscoring the importance of thoroughness in TB testing procedures.
Common mistakes
-
Leaving out essential information such as the healthcare professional's name or the testing location can lead to confusion and delays in processing the test results.
-
Failing to indicate the correct site (right or left) where the test was administered may result in an inaccurate record of the test.
-
Not recording the date placed or the date read can cause issues, especially since results need to be interpreted within 48-72 hours.
-
Overlooking the induration measurement in millimeters is a common mistake. This measurement is crucial for determining the test result.
-
Marking the PPD test result incorrectly can lead to a misunderstanding of the patient's status regarding tuberculosis.
-
Neglecting to obtain the signature of the healthcare professional who administered the test or read the results can render the form invalid.
Preview - Tb Test Form
|
|
|
|
|
TUBERCULOSISSKINTESTFORM |
||||||||
Healthcare Professional/Patient Name: |
|||||||||||||
Testing Location: |
|
|
|
|
|
|
|
|
|
|
|
||
Date Placed: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Site: |
Right |
Left |
|
|
|
|
|
|
|
|
|||
Lot #: |
|
|
|
|
|
Expiration Date: |
|
|
|||||
Signature (administered by): |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
RN |
|
MD Other: |
|
|
|
|||
Date Read (within |
|
|
|
|
|
|
|
Induration (please note in mm): |
|
mm |
|
PPD (Mantoux) Test Result: |
|
|
|
Negative |
Positive |
||
Signature (results read/reported by):
RN
MD Other:
*In order for this document to be valid/acceptable, all sections of this form must be completed.
Other PDF Templates
Acord Binder - The Acord 50 WM can influence the underwriting decisions of insurers.
When engaging in the sale or purchase of a mobile home, it is important to utilize a Missouri Mobile Home Bill of Sale, which serves as a formal record of the transaction. This document not only safeguards the rights of both buyer and seller but also provides clarity on the details of the sale, including important information about the mobile home itself. For those seeking a readily available form, consider using the Mobile Home Bill of Sale to facilitate the transfer process.
Odometer Statement Texas - This form is a vital component in protecting consumer rights in vehicle sales.
Bol Example - It is legally binding and outlines the obligations of the shipper and the carrier.
Documents used along the form
When dealing with tuberculosis testing, several additional forms and documents may accompany the TB Test form. Each serves a specific purpose in ensuring proper documentation and compliance with health regulations. Below is a list of commonly used forms.
- Patient Consent Form: This document ensures that the patient understands the TB test procedure and gives their permission for the test to be administered. It often includes information about potential risks and benefits.
- Nursing License Form: The AZ Forms Online provides essential resources for individuals seeking to navigate the requirements for obtaining or renewing their nursing license in Arizona, ensuring they meet all necessary legal guidelines.
- Medical History Questionnaire: This form gathers essential background information about the patient’s health. It may ask about previous TB exposure, vaccinations, and any current symptoms, helping healthcare providers assess risk factors.
- Follow-Up Care Plan: After a TB test, especially if results are positive, a follow-up care plan outlines the next steps for treatment or further testing. This document helps ensure the patient receives appropriate care and monitoring.
- Notification of Results Form: This form is used to communicate the results of the TB test to the patient and relevant healthcare providers. It ensures that all parties are informed and can take necessary actions based on the results.
- Employee Health Record: In workplace settings, this document tracks the health status of employees, including TB test results. It helps employers maintain a safe environment and comply with occupational health regulations.
Each of these documents plays a vital role in the TB testing process. They help facilitate communication, ensure informed consent, and promote proper follow-up care, ultimately contributing to the health and safety of individuals and communities.
Similar forms
The Tuberculosis Skin Test Form is similar to the Vaccination Record. Both documents serve to track an individual's health status regarding infectious diseases. The Vaccination Record details vaccinations received, including the type, date, and administering healthcare professional. Like the TB Test Form, it requires signatures from healthcare providers to confirm the administration and results, ensuring accountability and accuracy in health records.
Another comparable document is the Medical History Form. This form collects comprehensive information about a patient's past and present health conditions. It includes details on previous tests, treatments, and medications. Similar to the TB Test Form, it is essential for healthcare providers to have complete information to make informed decisions regarding patient care.
The Allergy Information Form is also akin to the TB Test Form. It documents any known allergies a patient may have, including reactions and severity. Both forms require signatures from healthcare professionals to validate the information provided. This ensures that medical personnel are aware of potential risks when treating patients.
The Laboratory Test Results Form shares similarities with the TB Test Form as well. It provides specific results from various tests conducted on a patient, including dates and interpretations. Just like the TB Test Form, it must be filled out completely and signed by the healthcare provider to be considered valid, ensuring that patients receive accurate information about their health status.
The Immunization Consent Form is another document that parallels the TB Test Form. This form is used to obtain a patient's consent for vaccinations, detailing the specific immunizations they will receive. Both forms require signatures from healthcare providers and patients, emphasizing the importance of informed consent in medical procedures.
The Health Screening Form also resembles the TB Test Form. It gathers information regarding a patient's overall health, including screenings for various conditions. Similar to the TB Test Form, it must be filled out thoroughly and signed by a healthcare professional, ensuring that all necessary information is recorded for effective patient management.
The Patient Intake Form is comparable as well. This document collects essential information about a new patient, including medical history, current medications, and reason for the visit. Like the TB Test Form, it requires completion of all sections and validation through signatures, which helps healthcare providers understand the patient’s background and needs better.
The Consent for Treatment Form shares characteristics with the TB Test Form. This document secures a patient's consent for medical treatment or procedures. Both forms necessitate signatures to confirm that patients understand the tests or treatments they are undergoing, reinforcing the importance of patient autonomy in healthcare.
Understanding the necessary paperwork is crucial when it comes to tenancy agreements. For example, the process involves acknowledging the legal implications of the Notice to Quit form for landlords and tenants, which serves as a formal notification regarding the termination of tenancy. This document outlines essential steps that landlords must follow to ensure compliance with legal standards.
Lastly, the Release of Medical Information Form is similar to the TB Test Form in that it allows patients to authorize the sharing of their health information with other parties. Like the TB Test Form, it must be completed and signed to ensure that all legal requirements are met, protecting patient confidentiality while facilitating necessary communication among healthcare providers.
Dos and Don'ts
When filling out the TB Test form, there are important dos and don'ts to keep in mind. Here is a helpful list:
- Do write clearly in all sections of the form.
- Do ensure that the date placed and date read are accurate.
- Do include the correct site of the test (right or left).
- Don't leave any sections blank; all fields must be completed.
- Don't forget to sign the form where required.
- Don't use abbreviations that might confuse the reader.
Key takeaways
Here are key takeaways about filling out and using the Tb Test form:
- Complete All Sections: Ensure that every part of the form is filled out. Incomplete forms may not be accepted.
- Patient Information: Clearly write the healthcare professional's name and the patient's name at the top of the form.
- Testing Location: Specify where the test is being conducted. This helps in tracking and record-keeping.
- Date Placed: Record the exact date when the test is administered. This is crucial for timing the reading of results.
- Induration Measurement: Measure the induration in millimeters (mm) and note it accurately. This measurement determines the test result.
- Reading the Results: The results must be read within 48-72 hours after placement. Make sure to adhere to this timeframe.
- Signature Requirement: Both the person administering the test and the one reading the results must sign the form. This adds validity to the document.
How to Use Tb Test
Completing the TB Test form is essential for documenting your test results accurately. Follow these steps carefully to ensure that all necessary information is recorded properly.
- Begin by entering the Healthcare Professional/Patient Name at the top of the form.
- Next, fill in the Testing Location where the test is being administered.
- Record the Date Placed, which is the date the test was given.
- Indicate the Site of the test, marking either the Right or Left arm.
- Write down the Lot # of the test used.
- Fill in the Expiration Date of the test.
- The Signature (administered by) section must be completed by the healthcare professional who administered the test. Choose from RN, MD, or Other.
- Leave space for the Date Read, which should be filled in within 48-72 hours from the date placed.
- Note the Induration measurement in millimeters (mm) in the designated area.
- Mark the PPD (Mantoux) Test Result as either Negative or Positive.
- Finally, the Signature (results read/reported by) must be filled in by the healthcare professional who read the results. Again, choose from RN, MD, or Other.
Ensure that all sections of the form are completed for it to be valid and acceptable. Once filled out, the form can be submitted as required.